Yonsei Med J.
2010 Jul;51(4):557-561. 10.3349/ymj.2010.51.4.557.
Cesium Implant for Tongue Carcinoma with a Thickness of 1.5 cm or More: Cases Successfully Treated with a Modified Manchester System
- Affiliations
-
- 1Department of Biomedical Sciences and Engineering, Faculty of Health Sciences, Graduate School of Health Sciences, Hokkaido University, Sapporo, Japan. trout@hs.hokudai.ac.jp
- 2Department of Oral Surgery, Keiyukai Sapporo Hospital, Sapporo, Japan.
- 3Department of Otolaryngology, Head and Neck Surgery, Hokkaido University Graduate School of Medicine, Sapporo, Japan.
- 4Oral Diagnosis and Medicine, Graduate School of Dental Medicine, Hokkaido University, Sapporo, Japan.
- 5Department of Dental Radiology, Graduate School of Dental Medicine, Hokkaido University Hospital, Sapporo, Japan.
- 6Department of Radiology, Graduate School of Medicine, Hokkaido University, Sapporo, Japan.
- 7Department of Radiology, Hokkaido Cancer Centre, Sapporo, Japan.
- KMID: 1805194
- DOI: http://doi.org/10.3349/ymj.2010.51.4.557
Abstract
- PURPOSE
Deciding on treatment carcinoma of the tongue when the tumor has a thickness of 1.5 cm or more is difficult. Surgery often requires wide resection and re-construction, leading to considerable functional impairment. A cesium implant is an attractive option, but according to the Manchester System, a two plane implant is needed.
MATERIALS AND METHODS
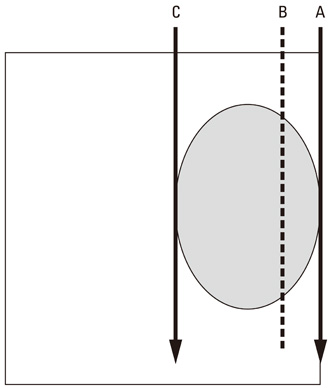
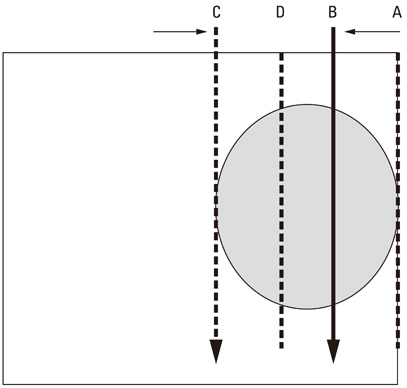
According to the textbook, a tumor is sandwiched between the needles, which are implanted at the edge of the tumor. This may cause an unnecessarily high dose to the outer surface of the tongue, which sometimes leads to a persistent ulcer. To avoid this complication, we invented a modified implantation method, and applied the method to five consecutive patients.
RESULTS
With a minimum follow-up of 2 years, all primary tumors in 5 consecutive patients have been controlled. No complications occurred in soft tissue of the tongue or in the mandible.
CONCLUSION
Our modified Manchester System was feasible and effective for tumors that has a thickness of 1.5 cm or more.
Figure
Reference
-
1. Duthie MB, Gupta NK, Pointon CS. Pointon RCS, editor. Head and neck. The radiotherapy of malignant disease. 1991. London: Springer-Verlag;156.
Article2. Hosokawa Y, Shirato H, Nishioka T, Tsuchiya K, Chang TC, Kagei K, et al. Effect of treatment time on outcome of radiotherapy for oral tongue carcinoma. Int J Radiat Oncol Biol Phys. 2003. 57:71–78.
Article3. Mendenhall WM, Riggs CE, Cassisi NJ. Devita VT, Hellman S, Rosenberg S, editors. Treatment of head and neck cancers. Cancer principle and practice of oncology. 2005. Philadelphia: Lippincott Williams and Wilkins;682.4. Obinata K, Ohmori K, Tuchiya K, Nishioka T, Shirato H, Nakamura M. Clinical study of a spacer to help prevent osteoradionecrosis resulting from brachytherapy for tongue cancer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003. 95:246–250.
Article5. O'Brien CJ, Lauer CS, Fredricks S, Clifford AR, McNeil EB, Bagia JS, et al. Tumor thickness influences prognosis of T1 and T2 oral cavity cancer--but what thickness? Head Neck. 2003. 25:937–945.6. Po Wing Yuen A, Lam KY, Lam LK, Ho CM, Wong A, Chow TL, et al. Prognostic factors of clinically stage I and II oral tongue carcinoma-A comparative study of stage, thickness, shape, growth pattern, invasive front malignancy grading, Martinez-Gimeno score, and pathologic features. Head Neck. 2002. 24:513–520.
Article7. Mukhija V, Gupta S, Jacobson AS, Anderson Eloy J, Genden EM. Selective neck dissection following adjuvant therapy for advanced head and neck cancer. Head Neck. 2009. 31:183–188.
Article8. Frank DK, Hu KS, Culliney BE, Persky MS, Nussbaum M, Schantz SP, et al. Planned neck dissection after concomitant radiochemotherapy for advanced head and neck cancer. Laryngoscope. 2005. 115:1015–1020.
Article9. van der Putten L, van den Broek GB, de Bree R, van den Brekel MW, Balm AJ, Hoebers FJ, et al. Effectiveness of salvage selective and modified radical neck dissection for regional pathologic lymphadenopathy after chemoradiation. Head Neck. 2009. In press.
Article10. van der Putten L, van den Broek GB, de Bree R, van den Brekel MW, Balm AJ, Hoebers FJ, et al. Effectiveness of salvage selective and modified radical neck dissection for regional pathologic lymphadenopathy after chemoradiation. Head Neck. 2009. 31:593–603.
Article11. Nishio M, Sakurai T, Kagami Y, Narimatsu N, Saito A, Hareyam M, et al. [Results of brachytherapy of tongue cancer]. Gan No Rinsho. 1986. 32:339–344.12. Urashima Y, Nakamura K, Kunitake N, Shioyama Y, Sasaki T, Ooga S, et al. Is glossectomy necessary for late nodal metastases without clinical local recurrence after initial brachytherapy for N0 tongue cancer? A retrospective experience in 111 patients who received salvage therapy for cervical failure. Jpn J Clin Oncol. 2006. 36:3–6.13. Hareyama M, Nishio M, Saito Y, Kagami Y, Asano K, Oouchi A, Narimatsu N, et al. Results of cesium needle interstitial implantation for carcinoma of the oral tongue. Int J Radiat Oncol Biol Phys. 1993. 25:29–34.
Article14. Nishioka T, Homma A, Furuta Y, Aoyama H, Suzuki F, Ohmori K, et al. A novel approach to advanced carcinoma of the tongue: cases successfully treated with combination of superselective intra-arterial chemotherapy and external/high-dose-rate interstitial radiotherapy. Jpn J Clin Oncol. 2006. 36:822–826.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Adeno-Squamous Cell Carcinoma at the Posterior Tongue via Median Glossotomy Approach
- Letter: Patient-Guided Improvements for Pediatric Obesity Services
- Assessment of Oropharyngeal Dysphagia in Patients With Parkinson Disease: Use of Ultrasonography
- A Case of Black Hairy Tongue
- Two Cases of Combined Geographic Tongue and Fissured Tongue in Generalized Pustular Psoriasis