Ann Surg Treat Res.
2015 Feb;88(2):100-105. 10.4174/astr.2015.88.2.100.
Effect of donor-specific antibodies and panel reactive antibodies in living donor liver transplant recipients
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. djjoo@yuhs.ac
- 2The Research Institute for Transplantation, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Surgery, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- KMID: 1804127
- DOI: http://doi.org/10.4174/astr.2015.88.2.100
Abstract
- PURPOSE
Preformed circulating donor-specific antibodies (DSAs) immunologically challenge vascular endothelium and the bile duct. However, the liver is an immune-tolerant organ and can avoid immunological challenges. This study was undertaken to analyze the effects of DSAs after adult living donor liver transplantation (LDLT).
METHODS
We retrospectively reviewed 219 LDLT patients' records treated at our center.
RESULTS
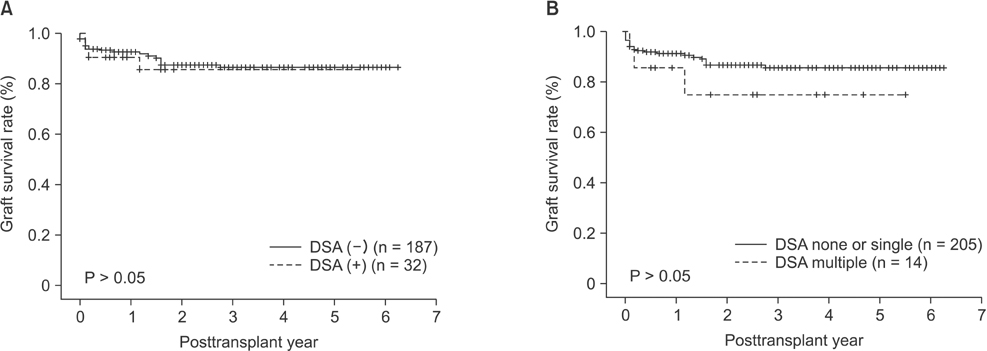
Of the 219 patients, 32 (14.6%) were DSA (+) and 187 (85.4%) were DSA (-). Class I DSAs were present in 18 patients, class II in seven patients, and both in seven patients. Seven patients (3.2%) showed DSA to HLA-A, four (1.8%) to HLA-B, seven (3.2%) to HLA-DR, and 14 (6.4%) to two or more HLAs. More DSAs were observed in female recipients than male recipients in the DSA (+) group. The DSA (+) group showed significantly higher levels of class I and II panel reactive antibody (PRA) than did the DSA (-) group. No significant intergroup differences were found between incidences of primary nonfunction, acute rejection, vascular complication, or biliary complication. There were no significant differences in graft survival rates between the two groups. However, the recipients with multiple DSAs tended to have more acute rejection episodes and events of biliary stricture and lower graft survival rates than did patients in the DSA (-) group.
CONCLUSION
In LDLT, the presence of multiple DSAs and high PRA seemed to be associated with poor graft outcomes, although our results did not reach statistical significance. Large cohort studies are necessary to clarify the impact of DSA and PRA in LDLT.
Keyword
MeSH Terms
-
Adult
Antibodies*
Bile Ducts
Cohort Studies
Constriction, Pathologic
Endothelium, Vascular
Female
Graft Survival
HLA-A Antigens
HLA-B Antigens
HLA-DR Antigens
Humans
Incidence
Liver Transplantation
Liver*
Living Donors*
Male
Retrospective Studies
Transplantation*
Transplants
Antibodies
HLA-A Antigens
HLA-B Antigens
HLA-DR Antigens
Figure
Reference
-
1. Hori T, Uemoto S, Takada Y, Oike F, Ogura Y, Ogawa K, et al. Does a positive lymphocyte cross-match contraindicate living-donor liver transplantation? Surgery. 2010; 147:840–844.2. Suehiro T, Shimada M, Kishikawa K, Shimura T, Soejima Y, Yoshizumi T, et al. Influence of HLA compatibility and lymphocyte cross-matching on acute cellular rejection following living donor adult liver transplantation. Liver Int. 2005; 25:1182–1188.3. Ratner LE, Hadley GA, Hanto DW, Mohanakumar T. Immunology of renal allograft rejection. Arch Pathol Lab Med. 1991; 115:283–287.4. Abu-Elmagd KM, Wu G, Costa G, Lunz J, Martin L, Koritsky DA, et al. Preformed and de novo donor specific antibodies in visceral transplantation: long-term outcome with special reference to the liver. Am J Transplant. 2012; 12:3047–3060.5. Pons JA, Revilla-Nuin B, Ramirez P, Baroja-Mazo A, Parrilla P. Development of immune tolerance in liver transplantation. Gastroenterol Hepatol. 2011; 34:155–169.6. Taner T, Gandhi MJ, Sanderson SO, Poterucha CR, De Goey SR, Stegall MD, et al. Prevalence, course and impact of HLA donor-specific antibodies in liver transplantation in the first year. Am J Transplant. 2012; 12:1504–1510.7. Sugawara Y, Makuuchi M, Kaneko J, Kishi Y, Hata S, Kokudo N. Positive T lymphocytotoxic cross-match in living donor liver transplantation. Liver Transpl. 2003; 9:1062–1066.8. Suh KS, Kim SB, Chang SH, Kim SH, Minn KW, Park MH, et al. Significance of positive cytotoxic cross-match in adult-to-adult living donor liver transplantation using small graft volume. Liver Transpl. 2002; 8:1109–1113.9. Joo DJ, Ju MK, Huh KH, Kim MS, Choi GH, Choi JS, et al. Does lymphocyte cross-matching predict acute rejection and graft survival in liver transplantation? Transplant Proc. 2012; 44:418–420.10. Matinlauri IH, Hockerstedt KA, Isoniemi HM. Equal overall rejection rate in pretransplant flow-cytometric cross-match negative and positive adult recipients in liver transplantation. Clin Transplant. 2005; 19:626–631.11. Heeger PS, Dinavahi R. Transplant immunology for non-immunologist. Mt Sinai J Med. 2012; 79:376–387.12. Wiesner RH, Demetris AJ, Belle SH, Seaberg EC, Lake JR, Zetterman RK, et al. Acute hepatic allograft rejection: incidence, risk factors, and impact on outcome. Hepatology. 1998; 28:638–645.13. Lan X, Zhang MM, Pu CL, Guo CB, Kang Q, Li YC, et al. Impact of human leukocyte antigen mismatching on outcomes of liver transplantation: a meta-analysis. World J Gastroenterol. 2010; 16:3457–3464.14. Everly MJ. Donor-specific anti-HLA antibody monitoring and removal in solid organ transplant recipients. Clin Transpl. 2011; 319–325.15. O'Leary JG, Klintmalm GB. Impact of donor-specific antibodies on results of liver transplantation. Curr Opin Organ Transplant. 2013; 18:279–284.16. O'Leary JG, Kaneku H, Jennings LW, Bañuelos N, Susskind BM, Terasaki PI, et al. Preformed class II donor-specific antibodies are associated with an increased risk of early rejection after liver transplantation. Liver Transpl. 2013; 19:973–980.17. Kaneku H, O'Leary JG, Banuelos N, Jennings LW, Susskind BM, Klintmalm GB, et al. De novo donor-specific HLA antibodies decrease patient and graft survival in liver transplant recipients. Am J Transplant. 2013; 13:1541–1548.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of preexisting human leukocyte antigen donor-specific antibodies especially human leukocyte antigen-DQ on kidney transplant outcome
- Decreasing the operation time of living donor liver transplantation in the era of laparoscopic living donor hepatectomy
- Liver retransplantation for adult recipients
- ABO-Incompatible Living Donor Liver Transplantation
- A Pilot Study of Calcineurin Inhibitors (CNIs) and Steroid Avoidance Immunosuppressive Protocol among Living Donor Kidney Transplant Recipients