Ann Surg Treat Res.
2015 Feb;88(2):63-68. 10.4174/astr.2015.88.2.63.
Predictive factors of central lymph node metastasis in papillary thyroid carcinoma
- Affiliations
-
- 1Department of Surgery, Chungnam National University College of Medicine, Daejeon, Korea. kimjr@cnu.ac.kr
- 2Department of Surgery, Konkuk University Chungju Hospital, Chungju, Korea.
- KMID: 1804122
- DOI: http://doi.org/10.4174/astr.2015.88.2.63
Abstract
- PURPOSE
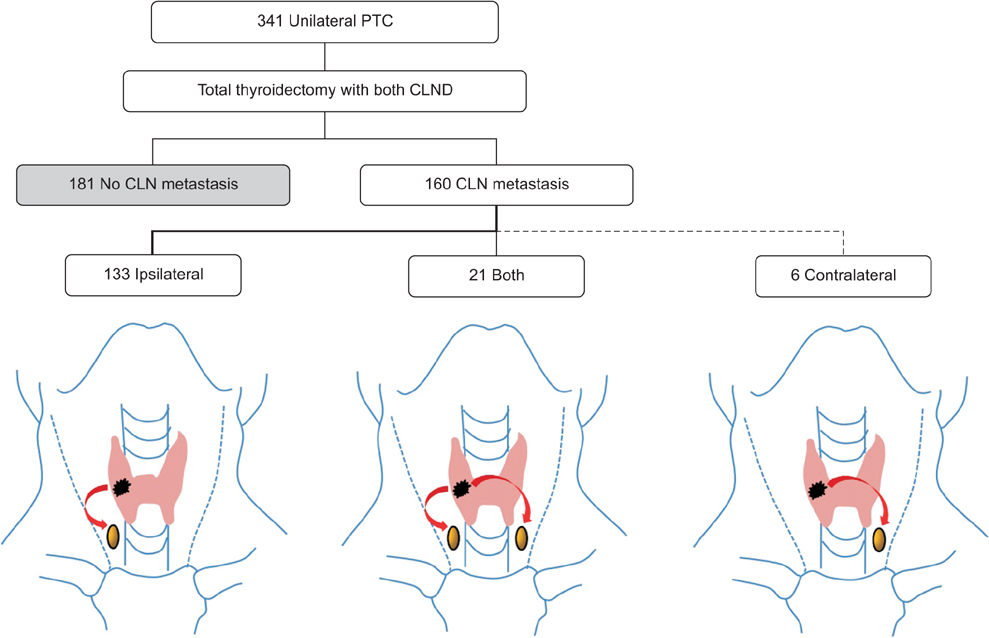
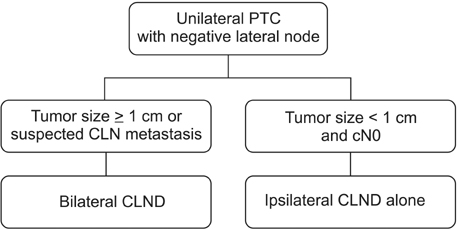
The aim of this study was to evaluate the correlation between central lymph node (CLN) metastasis and clinicopathologic characteristics of papillary thyroid cancer (PTC). In addition, we investigated the incidence and risk factors for contralateral CLN metastasis in unilateral PTC. This study suggests the appropriate surgical extent for CLN dissection.
METHODS
A prospective study of 500 patients with PTC who underwent total thyroidectomy and prophylactic bilateral CLN dissection was conducted.
RESULTS
Of 500 patients, 255 had CLN metastases. The rate of CLN metastasis was considerably higher in cases of younger patients (<45 years old) (P < 0.001; odds ratio [OR], 2.357) and of a maximal tumor size greater than 1 cm (P < 0.001; OR, 3.165). Ipsilateral CLN metastasis was detected in 83.1% of cases (133/160) of unilateral PTC, only contralateral CLN metastases in 3.7% of cases (6/160), and bilateral CLN metastases in 13.1% of cases (21/160). The rate of contralateral CLN metastasis was considerably higher in cases of PTC with a large tumor size (> or =1 cm) (P = 0.019; OR, 4.440) and with ipsilateral CLN metastasis (P = 0.047; OR, 2.613).
CONCLUSION
Younger age (<45 years old) and maximal tumor size greater than 1 cm were independent risk factors for CLN metastasis. Maximal tumor size greater than 1 cm and presence of ipsilateral CLN macrometastasis were independent risk factors for contralateral CLN metastasis. Therefore, both CLN dissections should be considered for unilateral PTC with a maximal tumor size greater than 1 cm or presence of ipsilateral CLN macrometastasis.
Keyword
MeSH Terms
Figure
Reference
-
1. Lundgren CI, Hall P, Dickman PW, Zedenius J. Clinically significant prognostic factors for differentiated thyroid carcinoma: a population-based, nested case-control study. Cancer. 2006; 106:524–531.2. Moo TA, McGill J, Allendorf J, Lee J, Fahey T 3rd, Zarnegar R. Impact of prophylactic central neck lymph node dissection on early recurrence in papillary thyroid carcinoma. World J Surg. 2010; 34:1187–1191.3. Shah JP, Loree TR, Dharker D, Strong EW, Begg C, Vlamis V. Prognostic factors in differentiated carcinoma of the thyroid gland. Am J Surg. 1992; 164:658–661.4. Scheumann GF, Gimm O, Wegener G, Hundeshagen H, Dralle H. Prognostic significance and surgical management of locoregional lymph node metastases in papillary thyroid cancer. World J Surg. 1994; 18:559–567.5. Mazzaferri EL, Jhiang SM. Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med. 1994; 97:418–428.6. Rossi RL, Cady B, Silverman ML, Wool MS, Horner TA. Current results of conservative surgery for differentiated thyroid carcinoma. World J Surg. 1986; 10:612–622.7. Lee YS, Kim SW, Kim SW, Kim SK, Kang HS, Lee ES, et al. Extent of routine central lymph node dissection with small papillary thyroid carcinoma. World J Surg. 2007; 31:1954–1959.8. Qubain SW, Nakano S, Baba M, Takao S, Aikou T. Distribution of lymph node micrometastasis in pN0 well-differentiated thyroid carcinoma. Surgery. 2002; 131:249–256.9. Lee J, Song Y, Soh EY. Central lymph node metastasis is an important prognostic factor in patients with papillary thyroid microcarcinoma. J Korean Med Sci. 2014; 29:48–52.10. Sugitani I, Fujimoto Y. Symptomatic versus asymptomatic papillary thyroid microcarcinoma: a retrospective analysis of surgical outcome and prognostic factors. Endocr J. 1999; 46:209–216.11. Sakorafas GH, Giotakis J, Stafyla V. Papillary thyroid microcarcinoma: a surgical perspective. Cancer Treat Rev. 2005; 31:423–438.12. Ito Y, Jikuzono T, Higashiyama T, Asahi S, Tomoda C, Takamura Y, et al. Clinical significance of lymph node metastasis of thyroid papillary carcinoma located in one lobe. World J Surg. 2006; 30:1821–1828.13. Gimm O, Rath FW, Dralle H. Pattern of lymph node metastases in papillary thyroid carcinoma. Br J Surg. 1998; 85:252–254.14. Moley JF, Lairmore TC, Doherty GM, Brunt LM, DeBenedetti MK. Preservation of the recurrent laryngeal nerves in thyroid and parathyroid reoperations. Surgery. 1999; 126:673–677.15. Kim MK, Mandel SH, Baloch Z, Livolsi VA, Langer JE, Didonato L, et al. Morbidity following central compartment reoperation for recurrent or persistent thyroid cancer. Arch Otolaryngol Head Neck Surg. 2004; 130:1214–1216.16. Hay ID, Hutchinson ME, Gonzalez-Losada T, McIver B, Reinalda ME, Grant CS, et al. Papillary thyroid microcarcinoma: a study of 900 cases observed in a 60-year period. Surgery. 2008; 144:980–987.17. Tisell LE, Nilsson B, Molne J, Hansson G, Fjalling M, Jansson S, et al. Improved survival of patients with papillary thyroid cancer after surgical microdissection. World J Surg. 1996; 20:854–859.18. Sywak M, Cornford L, Roach P, Stalberg P, Sidhu S, Delbridge L. Routine ipsilateral level VI lymphadenectomy reduces postoperative thyroglobulin levels in papillary thyroid cancer. Surgery. 2006; 140:1000–1005.19. Henry JF, Gramatica L, Denizot A, Kvachenyuk A, Puccini M, Defechereux T. Morbidity of prophylactic lymph node dissection in the central neck area in patients with papillary thyroid carcinoma. Langenbecks Arch Surg. 1998; 383:167–169.20. Goropoulos A, Karamoshos K, Christodoulou A, Ntitsias T, Paulou K, Samaras A, et al. Value of the cervical compartments in the surgical treatment of papillary thyroid carcinoma. World J Surg. 2004; 28:1275–1281.21. Gemsenjager E, Perren A, Seifert B, Schuler G, Schweizer I, Heitz PU. Lymph node surgery in papillary thyroid carcinoma. J Am Coll Surg. 2003; 197:182–190.22. Shindo M, Wu JC, Park EE, Tanzella F. The importance of central compartment elective lymph node excision in the staging and treatment of papillary thyroid cancer. Arch Otolaryngol Head Neck Surg. 2006; 132:650–654.23. Vergez S, Sarini J, Percodani J, Serrano E, Caron P. Lymph node management in clinically node-negative patients with papillary thyroid carcinoma. Eur J Surg Oncol. 2010; 36:777–782.24. Choi YJ, Yun JS, Kook SH, Jung EC, Park YL. Clinical and imaging assessment of cervical lymph node metastasis in papillary thyroid carcinomas. World J Surg. 2010; 34:1494–1499.25. Pellegriti G, Scollo C, Lumera G, Regalbuto C, Vigneri R, Belfiore A. Clinical behavior and outcome of papillary thyroid cancers smaller than 1.5 cm in diameter: study of 299 cases. J Clin Endocrinol Metab. 2004; 89:3713–3720.26. Pereira JA, Jimeno J, Miquel J, Iglesias M, Munne A, Sancho JJ, et al. Nodal yield, morbidity, and recurrence after central neck dissection for papillary thyroid carcinoma. Surgery. 2005; 138:1095–1100.27. Mirallié E, Visset J, Sagan C, Hamy A, Le Bodic MF, Paineau J. Localization of cervical node metastasis of papillary thyroid carcinoma. World J Surg. 1999; 23:970–973.28. Machens A, Hinze R, Thomusch O, Dralle H. Pattern of nodal metastasis for primary and reoperative thyroid cancer. World J Surg. 2002; 26:22–28.29. Wada N, Duh QY, Sugino K, Iwasaki H, Kameyama K, Mimura T, et al. Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg. 2003; 237:399–407.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidence and Predictive Factors of Central Neck Node Metastasis in Patients with T1, T2 Papillary Thyroid Cancer
- Retropharyngeal Lymph Node Metastasis of Thyroid Papillary Carcinoma
- Retropharyngeal Lymph Node Metastasis from Thyroid Papillary Carcinoma with Airway Obstruction
- Feasibility of Sentinel Lymph Node Biopsy in Papillary Thyroid Carcinoma
- The Pattern of Cervical Lymph Node Metastases in Papillary Thyroid Cancer