Yonsei Med J.
2013 Nov;54(6):1370-1376. 10.3349/ymj.2013.54.6.1370.
Perioperative Nutritional Status Changes in Gastrointestinal Cancer Patients
- Affiliations
-
- 1Department of Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 2Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. jakii@yuhs.ac
- 3Severance Hospital Nutritional Support Team, Seoul, Korea.
- 4Department of Nutrition and Dietetics, Severance Hospital, Yonsei University Health System, Seoul, Korea.
- KMID: 1798132
- DOI: http://doi.org/10.3349/ymj.2013.54.6.1370
Abstract
- PURPOSE
The presence of gastrointestinal (GI) cancer and its treatment might aggravate patient nutritional status. Malnutrition is one of the major factors affecting the postoperative course. We evaluated changes in perioperative nutritional status and risk factors of postoperative severe malnutrition in the GI cancer patients.
MATERIALS AND METHODS
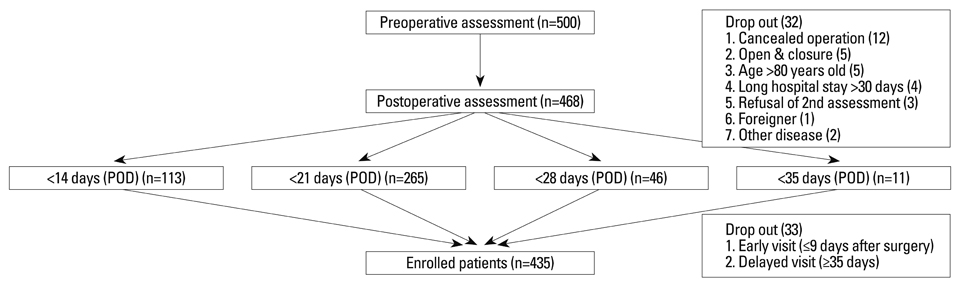
Nutritional status was prospectively evaluated using patient-generated subjective global assessment (PG-SGA) perioperatively between May and September 2011.
RESULTS
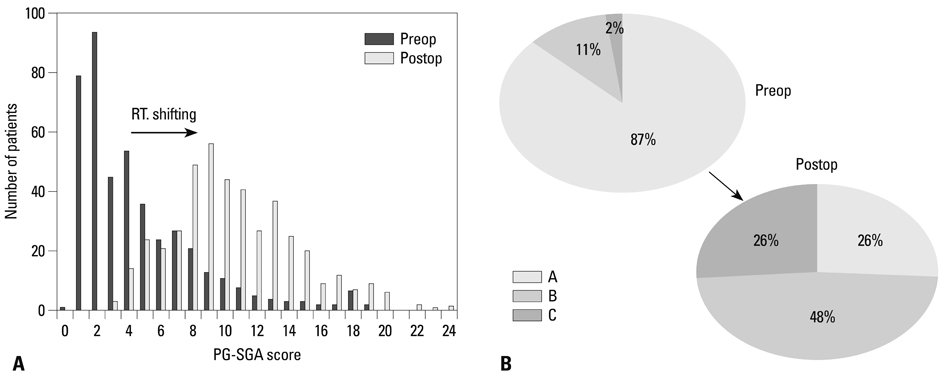
A total of 435 patients were enrolled. Among them, 279 patients had been diagnosed with gastric cancer and 156 with colorectal cancer. Minimal invasive surgery was performed in 225 patients. PG-SGA score increased from 4.5 preoperatively to 10.6 postoperatively (p<0.001). Ten patients (2.3%) were severely malnourished preoperatively, increasing to 115 patients (26.3%) postoperatively. In gastric cancer patients, postoperative severe malnourishment increased significantly (p<0.006). In univariate analysis, old age (>60, p<0.001), male sex (p=0.020), preoperative weight loss (p=0.008), gastric cancer (p<0.001), and open surgery (p<0.001) were indicated as risk factors of postoperative severe malnutrition. In multivariate analysis, old age, preoperative weight loss, gastric cancer, and open surgery remained significant as risk factors of severe malnutrition.
CONCLUSION
The prevalence of severe malnutrition among GI cancer patients in this study increased from 2.3% preoperatively to 26.3% after an operation. Old age, preoperative weight loss, gastric cancer, and open surgery were shown to be risk factors of postoperative severe malnutrition. In patients at high risk of postoperative severe malnutrition, adequate nutritional support should be considered.
MeSH Terms
Figure
Cited by 1 articles
-
Differences in the Survival of Gastric Cancer Patients after Gastrectomy according to the Medical Insurance Status
Jae Seong Jang, Dong Gue Shin, Hye Min Cho, Yujin Kwon, Dong Hui Cho, Kyung Bok Lee, Sang Soo Park, Jin Yoon, Yong Seog Jang, Il Myung Kim
J Gastric Cancer. 2013;13(4):247-254. doi: 10.5230/jgc.2013.13.4.247.
Reference
-
1. Bozzetti F, Gianotti L, Braga M, Di Carlo V, Mariani L. Postoperative complications in gastrointestinal cancer patients: the joint role of the nutritional status and the nutritional support. Clin Nutr. 2007; 26:698–709.
Article2. Garth AK, Newsome CM, Simmance N, Crowe TC. Nutritional status, nutrition practices and post-operative complications in patients with gastrointestinal cancer. J Hum Nutr Diet. 2010; 23:393–401.
Article3. Rey-Ferro M, Castaño R, Orozco O, Serna A, Moreno A. Nutritional and immunologic evaluation of patients with gastric cancer before and after surgery. Nutrition. 1997; 13:878–881.
Article4. Dzieniszewski J, Jarosz M, Szczygieł B, Długosz J, Marlicz K, Linke K, et al. Nutritional status of patients hospitalised in Poland. Eur J Clin Nutr. 2005; 59:552–560.
Article5. Pham NV, Cox-Reijven PL, Wodzig WK, Greve JW, Soeters PB. SGA and measures for muscle mass and strength in surgical Vietnamese patients. Nutrition. 2007; 23:283–291.
Article6. Waitzberg DL, Caiaffa WT, Correia MI. Hospital malnutrition: the Brazilian national survey (IBRANUTRI): a study of 4000 patients. Nutrition. 2001; 17:573–580.
Article7. Correia MI, Campos AC. ELAN Cooperative Study. Prevalence of hospital malnutrition in Latin America: the multicenter ELAN study. Nutrition. 2003; 19:823–825.
Article8. Naber TH, Schermer T, de Bree A, Nusteling K, Eggink L, Kruimel JW, et al. Prevalence of malnutrition in nonsurgical hospitalized patients and its association with disease complications. Am J Clin Nutr. 1997; 66:1232–1239.
Article9. Bozzetti F. SCRINIO Working Group. Screening the nutritional status in oncology: a preliminary report on 1,000 outpatients. Support Care Cancer. 2009; 17:279–284.
Article10. Ollenschläger G, Viell B, Thomas W, Konkol K, Bürger B. Tumor anorexia: causes, assessment, treatment. Recent Results Cancer Res. 1991; 121:249–259.
Article11. Braga M, Ljungqvist O, Soeters P, Fearon K, Weimann A, Bozzetti F, et al. ESPEN Guidelines on Parenteral Nutrition: surgery. Clin Nutr. 2009; 28:378–386.
Article12. Weimann A, Braga M, Harsanyi L, Laviano A, Ljungqvist O, Soeters P, et al. ESPEN Guidelines on Enteral Nutrition: Surgery including organ transplantation. Clin Nutr. 2006; 25:224–244.
Article13. Bauer J, Capra S, Ferguson M. Use of the scored Patient-Generated Subjective Global Assessment (PG-SGA) as a nutrition assessment tool in patients with cancer. Eur J Clin Nutr. 2002; 56:779–785.
Article14. Oh CA, Kim DH, Oh SJ, Choi MG, Noh JH, Sohn TS, et al. Changes of the preoperative and postoperative nutritional statuses in patients with gastric cancer and assessment of the nutritional factors that are correlated with short-term postoperative complications. J Korean Gastric Cancer Assoc. 2010; 10:5–12.
Article15. Ryu SW, Kim IH. Comparison of different nutritional assessments in detecting malnutrition among gastric cancer patients. World J Gastroenterol. 2010; 16:3310–3317.
Article16. Guo W, Ou G, Li X, Huang J, Liu J, Wei H. Screening of the nutritional risk of patients with gastric carcinoma before operation by NRS 2002 and its relationship with postoperative results. J Gastroenterol Hepatol. 2010; 25:800–803.
Article17. Ryan AM, Healy LA, Power DG, Rowley SP, Reynolds JV. Short-term nutritional implications of total gastrectomy for malignancy, and the impact of parenteral nutritional support. Clin Nutr. 2007; 26:718–727.
Article18. Kiyama T, Mizutani T, Okuda T, Fujita I, Tokunaga A, Tajiri T, et al. Postoperative changes in body composition after gastrectomy. J Gastrointest Surg. 2005; 9:313–319.
Article19. Abdiev S, Kodera Y, Fujiwara M, Koike M, Nakayama G, Ohashi N, et al. Nutritional recovery after open and laparoscopic gastrectomies. Gastric Cancer. 2011; 14:144–149.
Article20. Huhmann MB, August DA. Review of American Society for Parenteral and Enteral Nutrition (ASPEN) Clinical Guidelines for Nutrition Support in Cancer Patients: nutrition screening and assessment. Nutr Clin Pract. 2008; 23:182–188.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nutritional Assessment and Perioperative Nutritional Support in Gastric Cancer Patients
- Perioperative Nutritional Management in Cardiac Surgery
- Nutritional treatment after gastrectomy
- Perioperative nutritional therapy for surgical patients
- Perioperative outcomes of older adult patients with pancreatic cancer based on nutritional status: a retrospective cohorat study