J Korean Med Sci.
2009 Feb;24(1):57-61. 10.3346/jkms.2009.24.1.57.
Transcatheter Arterial Embolization Therapy for a Massive Polycystic Liver in Autosomal Dominant Polycystic Kidney Disease Patients
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Nephrology, College of Medicine, Kyunghee University, Seoul, Korea.
- 3Department of Radiology, Seoul National University College of Medicine, Seoul, Korea.
- 4Transplantation Research Institute, Seoul National University, Seoul, Korea.
- 5Cancer Research Institute?? Seoul National University, Seoul, Korea.
- 6Department of Internal Medicine, Eulji General Hospital, Eulji University, Seoul, Korea. ondahl@yahoo.com
- KMID: 1794407
- DOI: http://doi.org/10.3346/jkms.2009.24.1.57
Abstract
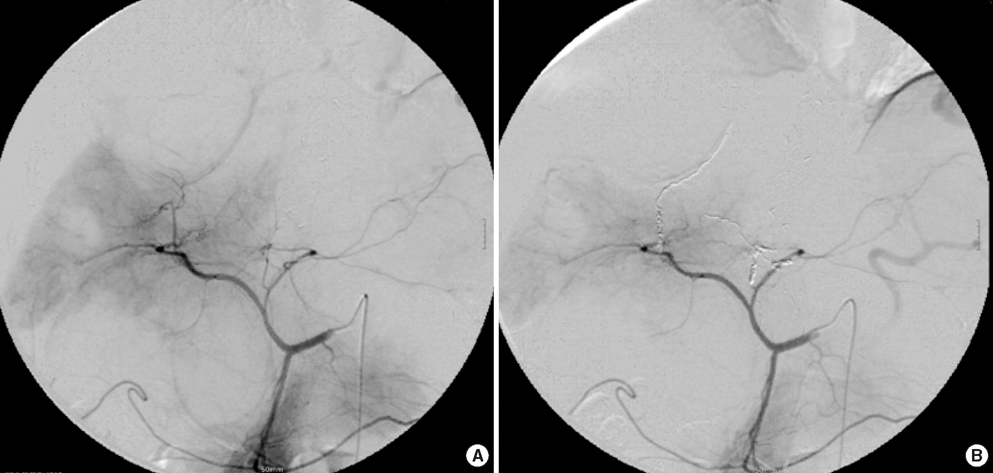
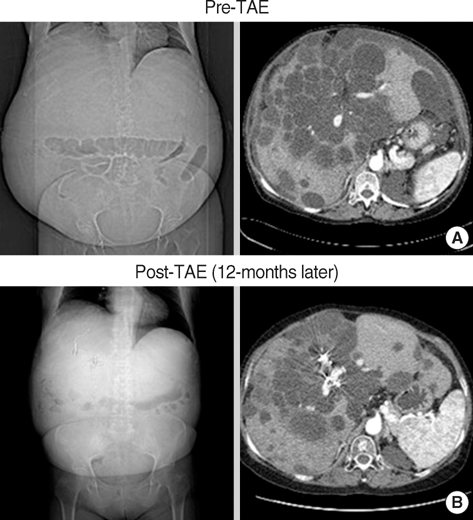
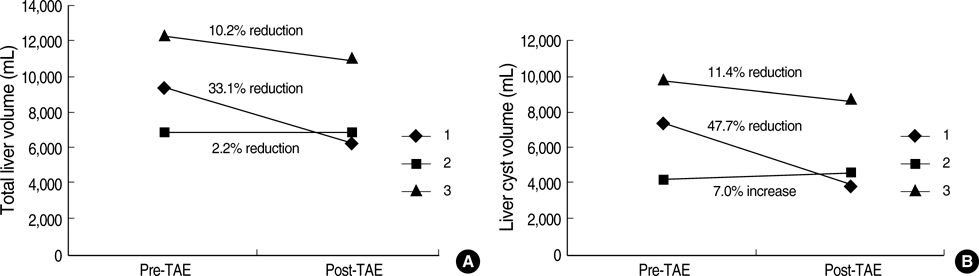
- Polycystic liver is the most common extra-renal manifestation associated with autosomal dominant polycystic kidney disease (ADPKD), comprising up to 80% of all features. Patients with polycystic liver often suffer from abdominal discomfort, dyspepsia, or dyspnea; however, there have been few ways to relieve their symptoms effectively and safely. Therefore, we tried transcatheter arterial embolization (TAE), which has been used in treating hepatocellular carcinoma. We enrolled four patients with ADPKD in Seoul National University Hospital, suffering from enlarged polycystic liver. We embolized the hepatic arteries supplying the dominant hepatic segments replaced by cysts using polyvinyl alcohol particles and micro-coils. The patients were evaluated 12 months after embolization for the change in both liver and cyst volumes. Among four patients, one patient was lost in follow up and 3 patients were included in the analysis. Both liver (33%; 10%) and cyst volume (47.7%; 11.4%) substantially decreased in two patients. Common adverse events were fever, epigastric pain, nausea, and vomiting. We suggest that TAE is effective and safe in treating symptomatic polycystic liver in selected ADPKD patients.
MeSH Terms
Figure
Reference
-
1. Hwang DY, Ahn C, Lee JG, Lee EJ, Cho JT, Hwang YH, Eo HS, Chae HJ, Kim SJ, Kim Y, Han JS, Kim S, Lee JS, Kim SH. Hepatic complications in autosomal-dominant polycystic kidney disease. 20th Annual Spring Conference of Korean Society of Nephrology. 2000. 19:Seoul, Korea. S306.2. Chauveau D, Fakhouri F, Grunfeld JP. Liver involvement in autosomal-dominant polycystic kidney disease: therapeutic dilemma. J Am Soc Nephrol. 2000. 11:1767–1775.3. Erdogan D, van Delden OM, Rauws EA, Busch OR, Lameris JS, Gouma DJ, van Gulik TM. Results of percutaneous sclerotherapy and surgical treatment in patients with symptomatic simple liver cysts and polycystic liver disease. World J Gastroenterol. 2007. 13:3095–3100.
Article4. Robinson TN, Stiegmann GV, Everson GT. Laparoscopic palliation of polycystic liver disease. Surg Endosc. 2005. 19:130–132.
Article5. Arnold HL, Harrison SA. New advances in evaluation and management of patients with polycystic liver disease. Am J Gastroenterol. 2005. 100:2569–2582.
Article6. Takei R, Ubara Y, Hoshino J, Higa Y, Suwabe T, Sogawa Y, Nomura K, Nakanishi S, Sawa N, Katori H, Takemoto F, Hara S, Takaichi K. Percutaneous transcatheter hepatic artery embolization for liver cysts in autosomal dominant polycystic kidney disease. Am J Kidney Dis. 2007. 49:744–752.
Article7. Ubara Y, Takei R, Hoshino J, Tagami T, Sawa N, Yokota M, Katori H, Takemoto F, Hara S, Takaichi K. Intravascular embolization therapy in a patient with an enlarged polycystic liver. Am J Kidney Dis. 2004. 43:733–738.
Article8. Ubara Y. New therapeutic option for autosomal dominant polycystic kidney disease patients with enlarged kidney and liver. Ther Apher Dial. 2006. 10:333–341.
Article9. Sherstha R, McKinley C, Russ P, Scherzinger A, Bronner T, Showalter R, Everson GT. Postmenopausal estrogen therapy selectively stimulates hepatic enlargement in women with autosomal dominant polycystic kidney disease. Hepatology. 1997. 26:1282–1286.
Article10. Torres VE. Treatment of polycystic liver disease: one size does not fit all. Am J Kidney Dis. 2007. 49:725–728.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transcatheter Arterial Embolization Using Ethanol in a Dialysis Patient for Contracting Enlarged Polycystic Kidneys
- A Case of Renal Cell Carcinoma in Autosomal Dominant Polycystic Kidney Disease Hemodialyzed
- Autosomal Dominant Polycystic Kidney Disease: 2009 Update for Internists
- A Case of Transitional Cell Carcinoma Associated with Adult Polycystic Kidney Disease
- A Case of Dilated Cardiomyopathy Associated with Autosomal Dominant Polycystic Kidney Disease