Yonsei Med J.
2008 Aug;49(4):615-619. 10.3349/ymj.2008.49.4.615.
Endobronchial Tuberculosis Presenting as Right Middle Lobe Syndrome:Clinical Characteristics and Bronchoscopic Findings in 22 Cases
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, Gyeongsang National University, Jinju, Korea. hochkim@gshp.gsnu.ac.kr
- 2Department of Diagnostic Radiology, College of Medicine, Gyeongsang National University, Jinju, Korea.
- KMID: 1793197
- DOI: http://doi.org/10.3349/ymj.2008.49.4.615
Abstract
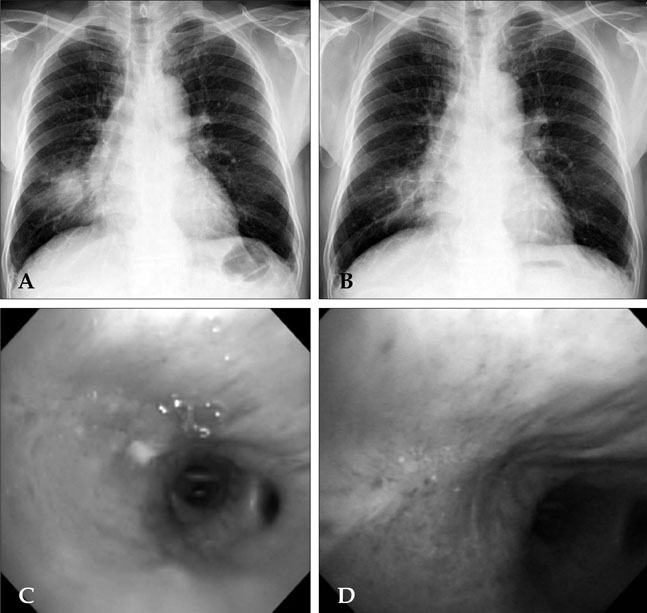
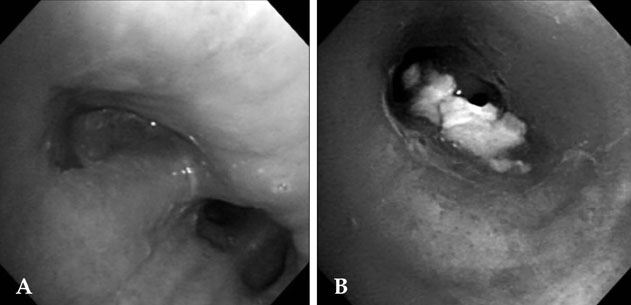
- PURPOSE
Endobronchial tuberculosis (EBTB) presenting as right middle lobe syndrome (RMLS) is an uncommon clinical condition. We investigated the clinical characteristics in patients with EBTB presenting as RMLS. PATIENTS and METHODS: We retrospectively reviewed the records of 22 patients with EBTB presenting as RMLS who were diagnosed at our hospital from 2003 to 2006. RESULTS: Its occurrence was more common in females than males (F, 18; M, 4). The mean age was 70.3 +/- 8.5 years, and 17 patients were above the age of 65 years. Cough with sputum was the most common manifestation and 2 patients were asymptomatic. In bronchoscopic analysis, the most common finding was edematous-type EBTB, which was found in 15 patients, followed by actively caseating type in 6 and tumorous type in 1. Acid-fast bacilli (AFB) staining for bronchial washing fluid was positive in only 5 patients: 1 with edematous type and 4 with actively caseating type. Bronchoscopic biopsy showed chronic granulomatous inflammation in 16 patients. Follow-up chest X-ray after treatment showed complete disappearance of the lesion in 2 patients, more than 50% improvement in 5, less than 50% improvement in 5, and no change of lesion in 4. CONCLUSION: Edematous-type EBTB was the most common type of EBTB presenting as RMLS, and it usually occurred in elderly patients. Culturing for mycobacterium and histologic examination by bronchoscopy are necessary for proper diagnosis in these patients.
MeSH Terms
Figure
Cited by 1 articles
-
Right middle lobe syndrome caused by eosinophilic mucoid impaction in adults
Ha Won Hwang, Joo-Hee Kim, Suk Yeon Kim, Sun Ho Lee, Soo Haeng Lee, Sunghoon Park, Yong Il Hwang, Seung Hun Jang, Ki-Suck Jung, In Jae Lee
Allergy Asthma Respir Dis. 2016;4(2):149-153. doi: 10.4168/aard.2016.4.2.149.
Reference
-
1. Chung HS. Endobronchial tuberculosis. J Korean Med Assoc. 2006. 49:799–805.
Article2. Gupta PP, Gupta KB, Agarwal D. Middle lobe syndrome due to tuberculous etiology: a series of 12 cases. Indian J Tuberc. 2006. 53:104–108.3. Gudmundsson G, Gross TJ. Middle lobe syndrome. Am Fam Physician. 1996. 53:2547–2550.4. Kwon KY, Myers JL, Swensen SJ, Colby TV. Middle lobe syndrome: a clinicopathological study of 21 patients. Hum Pathol. 1995. 26:302–307.
Article5. Kim HO, Ma JE, Lee SJ, Cho YJ, Jeong YY, Jeon KN, et al. Causes of Right Middle Lobe Syndrome: Recent Experience in Local Tertiary Hospital for Several Years. Tuberc Respir Dis. 2007. 62:192–196.6. Morrone N, Abe NS. Bronchoscopic finding in patients with pulmonary tuberculosis. J Bronchol. 2007. 14:15–18.7. An JY, Lee JE, Park HW, Lee JH, Yang SA, Jung SS, et al. Clinical and bronchoscopic features in endobronchial tuberculosis. Tuberc Respir Dis. 2006. 60:532–539.
Article8. Lee JH, Park SS, Lee DH, Shin DH, Yang SC, Yoo BM. Endobronchial tuberculosis: clinical and bronchoscopic features in 121 cases. Chest. 1992. 102:990–994.9. Chung HS, Lee JH, Han SK, Shim YS, Kim KY, Han YC, et al. Classification of endobronchial tuberculosis by the bronchoscopic fratures. Tuberc Respir Dis. 1991. 38:108–115.
Article10. Park EJ, Kim MO, Yang SC, Sohn JW, Yoon HJ, Shin DH, et al. Clinical and bronchoscopic features of 280 patients with endobronchial tuberculosis (1990-2001). Korean J Med. 2003. 64:284–292.11. Lee JY, Kim CM, Moon DS, Lee CW, Lee KS, Yang SC, et al. The clinical features of endobronchial tuberculosis - A retrospective study on 201 patients for 6 years. Tuberc Respir Dis. 1996. 43:671–682.
Article12. Kim HJ, Kim HS, Ma JE, Lee SJ, Ham HS, Cho YJ, et al. Clinical characteristics of endobronchial tuberculosis that develops in patients over 70 years of age. Tuberc Respir Dis. 2007. 63:412–416.
Article13. Chung HS, Lee JH. Bronchoscopic assessment of the evolution of endobronchial tuberculosis. Chest. 2000. 117:385–392.
Article14. Cisneros JR, Murray KM. Corticosteroids in tuberculosis. Ann Pharmacother. 1996. 30:1298–1303.
Article15. Rikimaru T. Therapeutic management of endobronchial tuberculosis. Expert Opin Pharmacother. 2004. 5:1463–1470.16. Park IW, Choi BW, Hue SH. Prospective study of corticosteroid as an adjunct in the treatment of endobronchial tuberculosis in adults. Respirology. 1997. 2:275–281.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Clinical Study of Middle Lobe Syndrome
- Changes in Bronchoscopic Findings during Treatment-Course in Active Endobronchial Tuberculosis
- Eosinophilic granulomatosis with polyangiitis presenting as an endobronchial nodule and atelectasis: A case report
- Flexible Bronchoscopic Observation on Endobronchial Tuberculosis
- A Clinical Study on Lesions in the Lingular Segment of the Left Upper Lobe