J Korean Med Sci.
2010 Jul;25(7):999-1004. 10.3346/jkms.2010.25.7.999.
Nosocomial Outbreak of Carbapenem-Resistant Acinetobacter baumannii in Intensive Care Units and Successful Outbreak Control Program
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea. pugae1@korea.ac.kr
- 2Department of Hospital Infection Control, Korea University Ansan Hospital, Ansan, Korea.
- 3Division of Intensive Care Unit, Korea University Ansan Hospital, Ansan, Korea.
- KMID: 1792947
- DOI: http://doi.org/10.3346/jkms.2010.25.7.999
Abstract
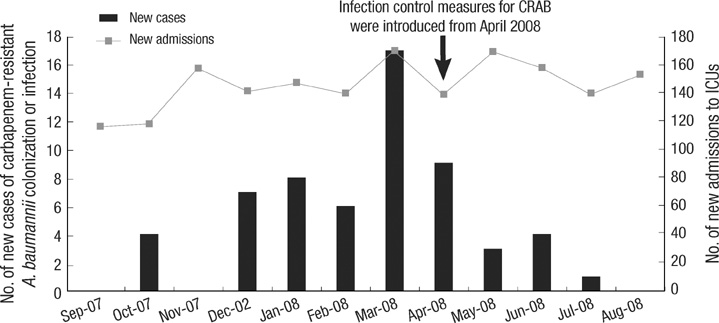
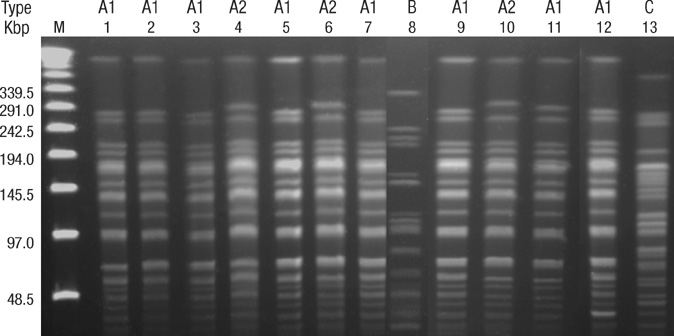
- Acinetobacter baumannii has been increasingly reported as a significant causative organism of various nosocomial infections. Here we describe an outbreak of carbapenem-resistant A. baumannii (CRAB) in the ICUs of a Korean university hospital, along with a successful outbreak control program. From October 2007 through July 2008, CRAB was isolated from 57 ICU patients. Nineteen patients were diagnosed as being truly infected with CRAB, four of whom were presumed to have died due to CRAB infection, producing a case-fatality rate of 21.1%. In surveillance of the environment and the healthcare workers (HCWs), CRAB was isolated from 24 (17.9%) of 135 environmental samples and seven (10.9%) of 65 HCWs. The pulsed field gel electrophoresis patterns showed that the isolates from patients, HCWs, and the environment were genetically related. Control of the outbreak was achieved by enforcing contact precautions, reducing environmental contamination through massive cleaning, and use of a closed-suctioning system. By August 2008 there were no new cases of CRAB in the ICUs. This study shows that the extensive spread of CRAB can happen through HCWs and the environmental contamination, and that proper strategies including strict contact precautions, massive environmental decontamination, and a closed-suctioning system can be effective for controlling CRAB outbreaks.
MeSH Terms
-
*Acinetobacter Infections/drug therapy/epidemiology/prevention & control
Acinetobacter baumannii/isolation & purification/metabolism/*pathogenicity
Adolescent
Adult
Aged
Aged, 80 and over
Anti-Bacterial Agents/*therapeutic use
Child
Child, Preschool
*Cross Infection/drug therapy/epidemiology/prevention & control
*Drug Resistance, Multiple, Bacterial
Hospitals, University
Humans
Infant
Infection Control/*methods
*Intensive Care Units
Korea/epidemiology
Male
Middle Aged
Young Adult
Figure
Reference
-
1. Cefai C, Richards J, Gould FK, McPeake P. An outbreak of Acinetobacter respiratory tract infection resulting from incomplete disinfection of ventilatory equipment. J Hosp Infect. 1990. 15:177–182.2. Siegman-Igra Y, Bar-Yosef S, Gorea A, Avram J. Nosocomial acinetobacter meningitis secondary to invasive procedures: report of 25 cases and review. Clin Infect Dis. 1993. 17:843–849.3. Kramer A, Schwebke I, Kampf G. How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infect Dis. 2006. 6:130.4. Aygun G, Demirkiran O, Utku T, Mete B, Urkmez S, Yilmaz M, Yasar H, Dikmen Y, Ozturk R. Environmental contamination during a carbapenem-resistant Acinetobacter baumannii outbreak in an intensive care unit. J Hosp Infect. 2002. 52:259–262.5. Levin AS, Gobara S, Mendes CM, Cursino MR, Sinto S. Environmental contamination by multidrug-resistant Acinetobacter baumannii in an intensive care unit. Infect Control Hosp Epidemiol. 2001. 22:717–720.6. Lee NY, Lee HC, Ko NY, Chang CM, Shih HI, Wu CJ, Ko WC. Clinical and economic impact of multidrug resistance in nosocomial Acinetobacter baumannii bacteremia. Infect Control Hosp Epidemiol. 2007. 28:713–719.7. Kwon KT, Oh WS, Song JH, Chang HH, Jung SI, Kim SW, Ryu SY, Heo ST, Jung DS, Rhee JY, Shin SY, Ko KS, Peck KR, Lee NY. Impact of imipenem resistance on mortality in patients with Acinetobacter bacteraemia. J Antimicrob Chemother. 2007. 59:525–530.8. Markogiannakis A, Fildisis G, Tsiplakou S, Ikonomidis A, Koutsoukou A, Pournaras S, Manolis EN, Baltopoulos G, Tsakris A. Cross-transmission of multidrug-resistant Acinetobacter baumannii clonal strains causing episodes of sepsis in a trauma intensive care unit. Infect Control Hosp Epidemiol. 2008. 29:410–417.9. Wybo I, Blommaert L, De Beer T, Soetens O, De Regt J, Lacor P, Pierard D, Lauwers S. Outbreak of multidrug-resistant Acinetobacter baumannii in a Belgian university hospital after transfer of patients from Greece. J Hosp Infect. 2007. 67:374–380.10. El Shafie SS, Alishaq M, Leni Garcia M. Investigation of an outbreak of multidrug-resistant Acinetobacter baumannii in trauma intensive care unit. J Hosp Infect. 2004. 56:101–105.11. Playford EG, Craig JC, Iredell JR. Carbapenem-resistant Acinetobacter baumannii in intensive care unit patients: risk factors for acquisition, infection and their consequences. J Hosp Infect. 2007. 65:204–211.12. Abbo A, Navon-Venezia S, Hammer-Muntz O, Krichali T, Siegman-Igra Y, Carmeli Y. Multidrug-resistant Acinetobacter baumannii. Emerg Infect Dis. 2005. 11:22–29.13. Zanetti G, Blanc DS, Federli I, Raffoul W, Petignat C, Maravic P, Francioli P, Berger MM. Importation of Acinetobacter baumannii into a burn unit: a recurrent outbreak of infection associated with widespread environmental contamination. Infect Control Hosp Epidemiol. 2007. 28:723–725.14. Simor AE, Lee M, Vearncombe M, Jones-Paul L, Barry C, Gomez M, Fish JS, Cartotto RC, Palmer R, Louie M. An outbreak due to multiresistant Acinetobacter baumannii in a burn unit: risk factors for acquisition and management. Infect Control Hosp Epidemiol. 2002. 23:261–267.15. Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections,1988. Am J Infect Control. 1988. 16:128–140.16. Yang JA, Park DW, Sohn JW, Yang IS, Kim KH, Kim MJ. Molecular analysis of isoleucyl-tRNA synthetase mutations in clinical isolates of methicillin-resistant Staphylococcus aureus with low-level mupirocin resistance. J Korean Med Sci. 2006. 21:827–832.17. Tenover FC, Arbeit RD, Goering RV, Mickelsen PA, Murray BE, Persing DH, Swaminathan B. Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol. 1995. 33:2233–2239.18. Zana S, Jarvis WR. Mayhall CG, editor. Investigations of outbreaks. Hospital epidemiology and infection control. 1996. Baltimore, MD: Williams & Wilkins;106–113.19. D'Agata EM, Thayer V, Schaffner W. An outbreak of Acinetobacter baumannii: the importance of cross-transmission. Infect Control Hosp Epidemiol. 2000. 21:588–591.20. Catalano M, Quelle LS, Jeric PE, Di Martino A, Maimone SM. Survival of Acinetobacter baumannii on bed rails during an outbreak and during sporadic cases. J Hosp Infect. 1999. 42:27–35.21. Wendt C, Dietze B, Dietz E, Ruden H. Survival of Acinetobacter baumannii on dry surfaces. J Clin Microbiol. 1997. 35:1394–1397.22. Siempos II, Vardakas KZ, Falagas ME. Closed tracheal suction systems for prevention of ventilator-associated pneumonia. Br J Anaesth. 2008. 100:299–306.23. Cobley M. Environmental contamination during tracheal suction - a comparison of disposable conventional catheters with a multiple-use closed system device anaesthesia. Anaesthesia. 1991. 46:957–961.24. Craven DE. Preventing ventilator-associated pneumonia in adults: sowing seeds of change. Chest. 2006. 130:251–260.25. Karageorgopoulos DE, Falagas ME. Current control and treatment of multidrug-resistant Acinetobacter baumannii infections. Lancet Infect Dis. 2008. 8:751–762.26. Rodriguez-Bano J, Cisneros JM, Fernandez-Cuenca F, Ribera A, Vila J, Pascual A, Martinez-Martinez L, Bou G, Pachon J. Clinical features and epidemiology of Acinetobacter baumannii colonization and infection in Spanish hospitals. Infect Control Hosp Epidemiol. 2004. 25:819–824.27. Marchaim D, Navon-Venezia S, Leavitt A, Chmelnitsky I, Schwaber MJ, Carmeli Y. Molecular and epidemiologic study of polyclonal outbreaks of multidrug-resistant Acinetobacter baumannii infection in an Israeli hospital. Infect Control Hosp Epidemiol. 2007. 28:945–950.28. Villers D, Espaze E, Coste-Burel M, Giauffret F, Ninin E, Nicolas F, Richet H. Nosocomial Acinetobacter baumannii infections: microbiological and clinical epidemiology. Ann Intern Med. 1998. 129:182–189.29. Braun G, Vidotto MC. Evaluation of adherence, hemagglutination, and presence of genes codifying for virulence factors of Acinetobacter baumannii causing urinary tract infection. Mem Inst Oswaldo Cruz. 2004. 99:839–844.30. Boujaafar N, Freney J, Bouvet PJ, Jeddi M. Cell surface hydrophobicity of 88 clinical strains of Acinetobacter baumannii. Res Microbiol. 1990. 141:477–482.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Analysis of Risk Factor and Infection Control of Carbapenem-Resistant Acinetobacter baumannii in a Medical Intensive Care Unit
- Update on the Epidemiology, Treatment, and Outcomes of Carbapenem-resistant Acinetobacter infections
- Nosocomial Infection by Sequence Type 357 Multidrug-Resistant Acinetobacter baumannii Isolates in a Neonatal Intensive Care Unit in Daejeon, Korea
- Clinical Characteristics of Intensive Care Unit Patients with Carbapenem Resistant Acinetobacter Baumannii Isolated from Sputum
- Multidrug-resistant Acinetobacter baumannii infection in the intensive care unit