J Korean Med Sci.
2010 Apr;25(4):552-556. 10.3346/jkms.2010.25.4.552.
Necessity of Radical Hysterectomy for Endometrial Cancer Patients with Cervical Invasion
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Seoul Metropolitan Boramae Hospital, Seoul, Korea.
- 2Department of Obstetrics and Gynecology, Seoul National University College of Medicine, Seoul, Korea. kjwksh@snu.ac.kr
- 3Department of Obstetrics and Gynecology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 4Department of Obstetrics and Gynecology, Yonsei University College of Medicine, Seoul, Korea.
- 5Department of Obstetrics and Gynecology, Cheil General Hospital and Women's Healthcare Center, Kwandong University College of Medicine, Seoul, Korea.
- 6Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University, School of Medicine, Seoul, Korea.
- 7Division of Gynecologic Oncology, University of Oklahoma, Oklahoma, USA.
- KMID: 1792924
- DOI: http://doi.org/10.3346/jkms.2010.25.4.552
Abstract
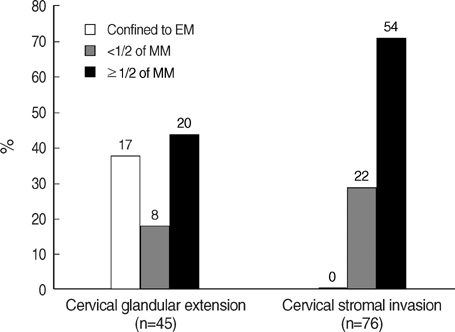
- To determine whether radical hysterectomy is necessary in the treatment of endometrial cancer patients with cervical involvement, we reviewed the medical records of women who underwent primary surgical treatment for endometrial carcinoma and selected patients with pathologically proven cervical invasion. Among 133 patients, 62 patients underwent extrafascial hysterectomy (EH) and 71 radical or modified radical hysterectomy (RH). The decision regarding EH or RH was made at the discretion of the attending surgeon. The sensitivity of pre-operative magnetic resonance imaging for cervical invasion was 44.7% (38/85). In RH patients, 10/71 (14.1%) patients had frankly histologic parametrial involvement (PMI). All were stage III or over. Eight of 10 patients had pelvic/paraaortic node metastasis and two showed extrauterine spread. In 74 patients with stage II cancer, RH was performed in 41 and PMI was not seen. Sixty-six (89.2%) patients had adjuvant radiation therapy and there were 3 patients who had developed recurrent disease in the RH group and none in the EH group (Mean follow-up: 51 months). Although these findings cannot conclusively refute or support the necessity of radical hysterectomy in patients with cervical extension, it is noteworthy that the risk of PMI seems to be minimal in patients with a tumor confined to the uterus without evidence of extrauterine spread.
MeSH Terms
-
Adult
Aged
Databases, Factual
Endometrial Neoplasms/epidemiology/*pathology/*surgery
Female
Humans
*Hysterectomy/methods
Korea/epidemiology
Middle Aged
Neoplasm Metastasis
Neoplasm Recurrence, Local/pathology
Neoplasm Staging
Radiotherapy, Adjuvant
Retrospective Studies
Treatment Outcome
Uterine Cervical Neoplasms/epidemiology/*pathology/*surgery
Figure
Cited by 1 articles
-
Treatment outcomes of patients with stage II pure endometrioid-type endometrial cancer: a Taiwanese Gynecologic Oncology Group (TGOG-2006) retrospective cohort study
Hung-Chun Fu, Jen-Ruei Chen, Min-Yu Chen, Keng-Fu Hsu, Wen-Fang Cheng, An-Jen Chiang, Yu-Min Ke, Yu-Chieh Chen, Yin-Yi Chang, Chia-Yen Huang, Chieh-Yi Kang, Yuan-Yee Kan, Sheng-Mou Hsiao, Ming-Shyen Yen
J Gynecol Oncol. 2018;29(5):. doi: 10.3802/jgo.2018.29.e76.
Reference
-
1. Korean Society of Obstetrics and Gynecology. Annual report of gynecologic cancer registry program in Korean for 2003 (Jan. 1st, 2003-Dec. 31st, 2003). Korean J Obstet Gynecol. 2006. 49:762–812.2. Niland JC. NCCN outcomes research database: data collection via the Internet. Oncology (Williston Park). 2000. 14:100–103.3. Elia G, Garfinkel DA, Goldberg GL, Davidson S, Runowicz CD. Surgical management of patients with endometrial cancer and cervical involvement. Eur J Gynaecol Oncol. 1995. 16:169–173.
Article4. Mannel RS, Berman ML, Walker JL, Manetta A, DiSaia PJ. Management of endometrial cancer with suspected cervical involvement. Obstet Gynecol. 1990. 75:1016–1022.
Article5. Leminen A, Forss M, Lehtovirta P. Endometrial adenocarcinoma with clinical evidence of cervical involvement: accuracy of diagnostic procedures, clinical course, and prognostic factors. Acta Obstet Gynecol Scand. 1995. 74:61–66.
Article6. Berman ML, Ballon SC, Lagasse LD, Watring WG. Prognosis and treatment of endometrial cancer. Am J Obstet Gynecol. 1980. 136:679–688.
Article7. Morrow CP, Di Saia PJ, Townsend DE. Current management of endometrial carcinoma. Obstet Gynecol. 1973. 42:399–406.8. Boronow RC, Morrow CP, Creasman WT, Disaia PJ, Silverberg SG, Miller A, Blessing JA. Surgical staging in endometrial cancer: clinical-pathologic findings of a prospective study. Obstet Gynecol. 1984. 63:825–832.9. Kadar N, Malfetano JH, Homesley HD. Determinants of survival of surgically staged patients with endometrial carcinoma histologically confined to the uterus: implications for therapy. Obstet Gynecol. 1992. 80:655–659.10. Wagenaar HC, Trimbos JB, Postema S, Anastasopoulou A, van der Geest RJ, Reiber JH, Kenter GG, Peters AA, Pattynama PM. Tumor diameter and volume assessed by magnetic resonance imaging in the prediction of outcome for invasive cervical cancer. Gynecol Oncol. 2001. 82:474–482.
Article11. Iwata S, Joja I, Okuno K, Miyagi Y, Sakaguchi Y, Kudo T, Hiraki Y. Cervical carcinoma with full-thickness stromal invasion: efficacy of dynamic MR imaging in the assessment of parametrial involvement. Radiat Med. 2002. 20:247–255.12. Rutledge F. The role of radical hysterectomy in adenocarcinoma of the endometrium. Gynecol Oncol. 1974. 2:331–347.
Article13. Watanabe Y, Aoki D, Kitagawa R, Takeuchi S, Sagae S, Sakuragi N, Yaegashi N. Disease Committee of Uterine Endometrial Cancer, Japanese Gynecologic Oncology Group. Status of surgical treatment procedures for endometrial cancer in Japan: Results of a Japanese Gynecologic Oncology Group Survey. Gynecol Oncol. 2007. 105:325–328.
Article14. Maggino T, Romagnolo C, Landoni F, Sartori E, Zola P, Gadducci A. An analysis of approaches to the management of endometrial cancer in North America: a CTF study. Gynecol Oncol. 1998. 68:274–279.
Article15. Danoff BF, McDay J, Louka M, Lewis GC, Lee J, Kramer S. Stage III Endometrial carcinoma: analysis of patterns of failure and therapeutic implications. Int J Radiat Oncol Biol Phys. 1980. 6:1491–1495.
Article16. Behbakht K, Yordan EL, Casey C, DeGeest K, Massad LS, Kirschner CV, Wilbanks GD. Prognostic indicators of survival in advanced endometrial cancer. Gynecol Oncol. 1994. 55:363–367.
Article17. Yura Y, Tauchi K, Koshiyama M, Yura S, Mori T, Matsushita K, Hayashi M, Yoshida M. Parametrial involvement in endometrial carcinomas: its incidence and correlation with other histological parameters. Gynecol Oncol. 1996. 63:114–119.
Article18. Masubuchi S, Fujimoto I, Masubuchi K. Lymph node metastasis and prognosis of endometrial carcinoma. Gynecol Oncol. 1979. 7:36–46.
Article19. Ambros RA, Kurman RJ. Combined assessment of vascular and myometrial invasion as a model to predict prognosis in stage I endometrioid adenocarcinoma of the uterine corpus. Cancer. 1992. 69:1424–1431.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A comparison of robot assisted and abdominal radical hysterectomy (RH) for early stage cervical and endometrial cancer
- Vaginal evisceration after radical hysterectomy and adjuvant radiation
- Cost-effectiveness analysis of simple hysterectomy compared to radical hysterectomy for early cervical cancer: analysis from the GCIG/CCTG CX.5/SHAPE trial
- The twenty-first century role of Piver-Rutledge type III radical hysterectomy and FIGO stage IA, IB1, and IB2 cervical cancer in the era of robotic surgery: a personal perspective
- Pelvic Drainage Following Radical Hysterectomy with Pelvic Lymphadenectomy for Cervical Cancer: Is it Necessary?