Korean J Gastroenterol.
2012 May;59(5):372-376. 10.4166/kjg.2012.59.5.372.
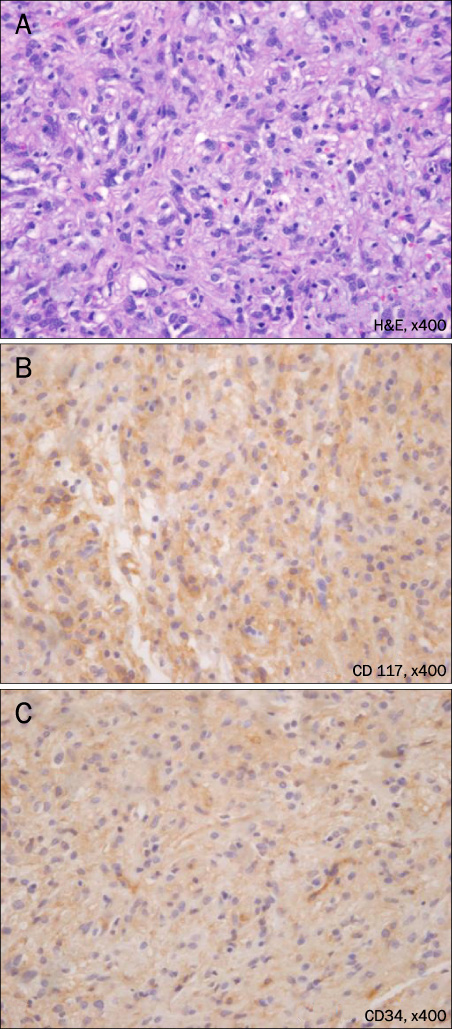
Gastroduodenal Intussusception Due to Pedunculated Polypoid Gastrointestinal Stromal Tumor
- Affiliations
-
- 1Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University College of Medicine, Seoul, Korea. Chongil.sohn@samsung.com
- KMID: 1792837
- DOI: http://doi.org/10.4166/kjg.2012.59.5.372
Abstract
- The gastrointestinal stromal tumor (GIST) is a mesenchymal tumor of the digestive tract showing differentiation along the line of interstitial cell of Cajal. The most GISTs in the stomach generally show the appearance of submucosal tumors. It is rare for GISTs to appear as a pedunculated polypoid lesion on endoscopy. We experienced a case of a 51-year-old man who had a pedunculated polypoid GIST. He was admitted to our hospital for nausea, vomiting, melena and severe anemia (hemoglobin 3.4 g/dL, hematocrit 10.8%). An upper endoscopy showed gastroduodenal intussusception due to a pedunculated polypoid mass. This report presents a rare case of endoscopically proven gastroduodenal intussusceptions due to pedunculated polypoid GIST in the stomach.
MeSH Terms
Figure
Reference
-
1. Nowain A, Bhakta H, Pais S, Kanel G, Verma S. Gastrointestinal stromal tumors: clinical profile, pathogenesis, treatment strategies and prognosis. J Gastroenterol Hepatol. 2005. 20:818–824.2. Hirota S, Isozaki K, Moriyama Y, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998. 279:577–580.3. Choi SH, Han JK, Kim SH, et al. Intussusception in adults: from stomach to rectum. AJR Am J Roentgenol. 2004. 183:691–698.4. Casali PG, Blay JY. Esmo/conticanet/eurobonet Consensus Panel of Experts. conticanet/eurobonet Consensus Panel of Experts. Gastrointestinal stromal tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010. 21:Suppl 5. v98–v102.5. Lanza FL, Graham DY, Nelson RS, Godines R, McKechnie JC. Endoscopic upper gastrointestinal polypectomy. Report of 73 polypectomies in 63 patients. Am J Gastroenterol. 1981. 75:345–348.6. Goenka MK, Bhasin DK, Singh V, et al. Gastric stromal tumor: treatment by snare polypectomy. Trop Gastroenterol. 1996. 17:43–46.7. Kim IH, Kim PS, Lee DH, et al. Gastric malignant stromal tumor with long stalk impacted into duodenum. Yonsei Med J. 1999. 40:510–513.8. Crowther KS, Wyld L, Yamani Q, Jacob G. Case report: gastroduodenal intussusception of a gastrointestinal stromal tumour. Br J Radiol. 2002. 75:987–989.9. Adjepong SE, Parameswaran R, Perry A, et al. Gastroduodenal intussusception due to gastrointestinal stromal tumor (GIST) treated by laparoscopic billroth II distal gastrectomy. Surg Laparosc Endosc Percutan Tech. 2006. 16:245–247.10. Tahara T, Shibata T, Nakamura M, et al. Gastrointestinal stromal tumor of the stomach with narrow stalk-like based, uneven protruding appearance presenting with severe acute anemia despite small size. Case Rep Gastroenterol. 2010. 4:111–117.11. Gupta P, Tewari M, Shukla HS. Gastrointestinal stromal tumor. Surg Oncol. 2008. 17:129–138.12. Lin F, Setya V, Signor W. Gastroduodenal intussusception secondary to a gastric lipoma: a case report and review of the literature. Am Surg. 1992. 58:772–774.13. Ha HK, Shinn KS, Kim IC, Bahk YW. Gastroduodenal intussusception due to a prolapsed gastric adenoma. AJR Am J Roentgenol. 1992. 159:432.14. Son JI, Lee JH, Lee SI, et al. A case of gastroduodenal intussusception secondary to gastric carcinoid tumor. Korean J Gastroenterol. 2001. 38:288–291.15. Lin JT. Endoscopic diagnosis of gastroduodenal intussusception. Endoscopy. 1996. 28:324.16. Miettinen M, Lasota J. Gastrointestinal stromal tumors: review on morphology, molecular pathology, prognosis, and differential diagnosis. Arch Pathol Lab Med. 2006. 130:1466–1478.17. Kang YK, Kim KM, Sohn T, et al. Korean GIST Study Group. Clinical practice guideline for accurate diagnosis and effective treatment of gastrointestinal stromal tumor in Korea. J Korean Med Sci. 2010. 25:1543–1552.18. Demetri GD, von Mehren M, Blanke CD, et al. Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med. 2002. 347:472–480.19. Ho MY, Blanke CD. Gastrointestinal stromal tumors: disease and treatment update. Gastroenterology. 2011. 140:1372–1376.20. Dematteo RP, Ballman KV, Antonescu CR, et al. American College of Surgeons Oncology Group (ACOSOG) Intergroup Adjuvant GIST Study Team. Adjuvant imatinib mesylate after resection of localised, primary gastrointestinal stromal tumour: a randomised, double-blind, placebo-controlled trial. Lancet. 2009. 373:1097–1104.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Gastroduodenal Intussusception Resulting from Large Hyperplastic Polyp
- Acute Pancreatitis and Gastroduodenal Intussusception Induced by an Underlying Gastric Gastrointestinal Stromal Tumor: A Case Report
- Gastroduodenal intussusception with pedunculated hamartoma
- Gastroduodenal intussusception of a gastrointestinal stromal tumor: a rare cause of acute pancreatitis
- Gastroduodenal Intussusception due to Gastric Submucosal Hemangiomatosis