Ann Pediatr Endocrinol Metab.
2015 Mar;20(1):34-39. 10.6065/apem.2015.20.1.34.
Etiologies and characteristics of children with chief complaint of short stature
- Affiliations
-
- 1Department of Pediatrics, Severance Children's Hospital, Yonsei University College of Medicine, Seoul, Korea. kimho@yuhs.ac
- 2Sowha Chidren's Hospital, Seoul, Korea.
- KMID: 1789529
- DOI: http://doi.org/10.6065/apem.2015.20.1.34
Abstract
- PURPOSE
Short stature is a very common reason for visits to pediatric endocrine clinics. It could be the first sign of an underlying disease. The purpose of this study is to investigate the etiologies and general characteristics of subjects who visited an outpatient clinic due to short stature.
METHODS
We retrospectively reviewed the medical records of 3,371 patients who visited Severance Children's Hospital with the chief complaint of short stature from 2010 to 2012. Medical history, auxological data, and laboratory tests including bone age were collected and analyzed. Chromosome studies or combined pituitary function tests were performed if needed.
RESULTS
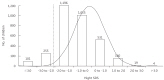
Approximately 89.4% of the subjects with the chief complaint of short stature who visited the outpatient clinic were of normal height, and only 10.6% of subjects were identified as having short stature. Of the subject of short stature, 44.7% were classified as having normal variant short stature; that is, familial short stature (23.0%), constitutional delay in growth (17.7%), and mixed form (3.9%). Pathological short stature was found in 193 subjects (54.2%). Among pathological short stature, most common etiology was growth hormone deficiency (GHD) (38.9%).
CONCLUSION
A majority of children had a normal height. Among children with short stature, pathological short stature and normal variants occupied a similar percentage. GHD was the most common cause of pathological short stature and found in about 20% of the children with short stature. In pathological short stature, the height, height velocity, and IGF-1 level were lower than in normal variants.
Keyword
MeSH Terms
Figure
Reference
-
1. Rieser PA. Educational, psychologic, and social aspects of short stature. J Pediatr Health Care. 1992; 6(5 Pt 2):325–332. PMID: 1453288.
Article2. Lechelt EC. Occupational affiliation and ratings of physical height and personal esteem. Psychol Rep. 1975; 36:943–946. PMID: 1144639.
Article3. Gordon M, Crouthamel C, Post EM, Richman RA. Psychosocial aspects of constitutional short stature: social competence, behavior problems, self-esteem, and family functioning. J Pediatr. 1982; 101:477–480. PMID: 7108676.
Article4. Stabler B, Clopper RR, Siegel PT, Stoppani C, Compton PG, Underwood LE. Academic achievement and psychological adjustment in short children. The National Cooperative Growth Study. J Dev Behav Pediatr. 1994; 15:1–6. PMID: 8195431.5. Sandberg DE, Voss LD. The psychosocial consequences of short stature: a review of the evidence. Best Pract Res Clin Endocrinol Metab. 2002; 16:449–463. PMID: 12464228.
Article6. Kranzler JH, Rosenbloom AL, Proctor B, Diamond FB Jr, Watson M. Is short stature a handicap? A comparison of the psychosocial functioning of referred and nonreferred children with normal short stature and children with normal stature. J Pediatr. 2000; 136:96–102. PMID: 10636982.
Article7. Allen DB, Cuttler L. Clinical practice. Short stature in childhood--challenges and choices. N Engl J Med. 2013; 368:1220–1228. PMID: 23534561.8. Ranke MB. The Kabi Pharmacia International Growth Study: aetiology classification list with comments. Acta Paediatr Scand Suppl. 1991; 379:87–92. PMID: 1815464.
Article9. Greulich W, Pyle S. Radiographic atlas of skeletal development of the hand and wrist. 2nd ed. Stanford: Stanford Iniversity Press;1959.10. Bayley N, Pinneau SR. Tables for predicting adult height from skeletal age: revised for use with the Greulich-Pyle hand standards. J Pediatr. 1952; 40:423–441. PMID: 14918032.
Article11. Kim JB, Yoo HW. Etiological classifications of children with chief complaint of short stature. J Korean Soc Pediatr Endocrinol. 1997; 2:1–9.12. Lashari SK, Korejo HB, Memon YM. To determine frequency of etiological factors in short statured patients presenting at an endocrine clinic of a tertiary care hospital. Pak J Med Sci. 2014; 30:858–861. PMID: 25097532.13. Papadimitriou A, Douros K, Papadimitriou DT, Kleanthous K, Karapanou O, Fretzayas A. Characteristics of the short children referred to an academic paediatric endocrine clinic in Greece. J Paediatr Child Health. 2012; 48:263–267. PMID: 22112203.
Article14. Lindsay R, Feldkamp M, Harris D, Robertson J, Rallison M. Utah Growth Study: growth standards and the prevalence of growth hormone deficiency. J Pediatr. 1994; 125:29–35. PMID: 8021781.
Article15. Zargar AH, Laway BA, Masoodi SR, Wani AI, Salahuddin M. An aetiological profile of short stature in the Indian subcontinent. J Paediatr Child Health. 1998; 34:571–576. PMID: 9928653.
Article16. Moayeri H, Aghighi Y. A prospective study of etiology of short stature in 426 short children and adolescents. Arch Iranian Med. 2004; 7:23–27.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Etiological Classifications of Children with Chief Complaint of Short Stature
- Approach to Short Stature in Children and Adolescent
- Comparison of Body Image, Self-Esteem and Behavior Problems between Children of Short and Normal Stature
- Deciphering short stature in children
- The Short Stature in Children with Hypertrophy of Adenoid and Tonsil or Allergic Rhinitis