J Korean Med Sci.
2013 Apr;28(4):555-563. 10.3346/jkms.2013.28.4.555.
Elevation of Morning Blood Pressure in Sodium Resistant Subjects by High Sodium Diet
- Affiliations
-
- 1Cardiovascular Center, Dongguk University Ilsan Hospital, Goyang, Korea. mooyong_rhee@dumc.or.kr
- 2Clinical Trial Center, Dongguk University Ilsan Hospital, Goyang, Korea.
- 3Division of Nephrology, Dongguk University Ilsan Hospital, Goyang, Korea.
- 4Department of Family Medicine, Dongguk University Ilsan Hospital, Goyang, Korea.
- 5Department of Food and Nutrition, Hanyang University, Seoul, Korea.
- 6Nutrition Policy Office, Food Safety Bureau, Korea Food and Drug Administration, Cheongwon, Korea.
- 7Department of Food & Nutrition Industry, Korea Health Industry Development Institute, Cheongwon, Korea.
- 8Department of Endocrinology and Metabolism, Sungkyunkwan University School of Medicine, Kangbuk Samsung Hospital, Seoul, Korea.
- 9Department of Statistics, Survey Research Center, Dongguk University, Seoul, Korea.
- KMID: 1786963
- DOI: http://doi.org/10.3346/jkms.2013.28.4.555
Abstract
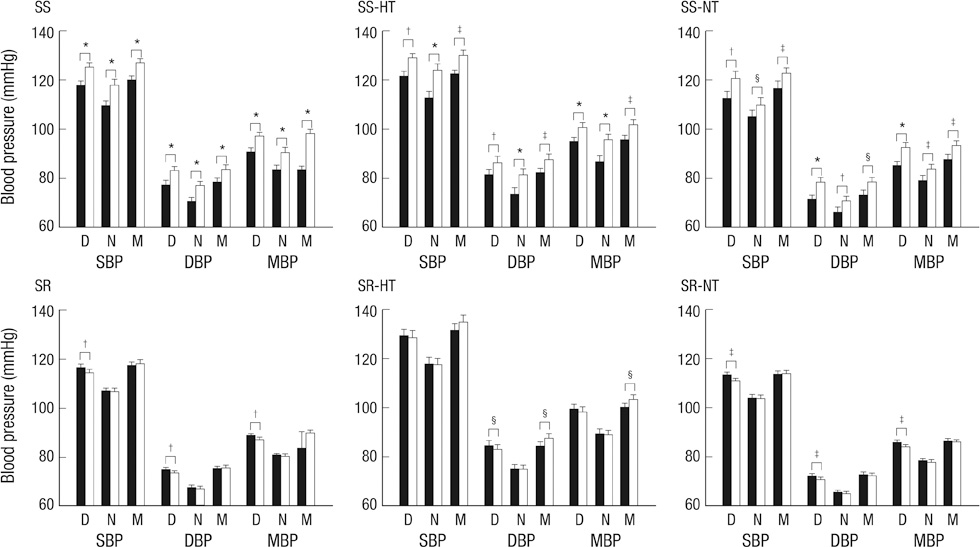
- The present study evaluated the response of blood pressure (BP) by dietary sodium in sodium resistant (SR) subjects. One hundred one subjects (mean age, 46.0 yr; 31 hypertensives) were admitted and given low sodium-dietary approaches to stop hypertension (DASH) diet (LSD, 100 mM NaCl/day) for 7 days and high sodium-DASH diet (HSD, 300 mM NaCl/day) for the following 7 days. On the last day of each diet, 24 hr ambulatory BP was measured. Morning systolic BP (SBP) and diastolic BP (DBP) were elevated after HSD in all subjects (P < 0.01), but daytime SBP and DBP were not changed (P > 0.05). In hypertensive subjects, morning DBP elevation was greater than daytime DBP elevation (P = 0.036), although both DBPs were significantly elevated after HSD. The augmented elevation of morning DBP in hypertensive subjects was contributed by the absolute elevation of morning DBP (P = 0.032) and relative elevation to daytime DBP (P = 0.005) in sodium resistant (SR) subjects, but not by sodium sensitive subjects. Although there was no absolute elevation, SR subjects with normotension showed a relative elevation of morning SBP compared to daytime SBP change after HSD (P = 0.009). The present study demonstrates an absolute and relative elevation of morning BP in SR subjects by HSD.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Elevation of heart-femoral pulse wave velocity by short-term low sodium diet followed by high sodium diet in hypertensive patients with sodium sensitivity
Moo-Yong Rhee, Ji-Hyun Kim, Sang-Hoon Na, Jin-Wook Chung, Jun-Ho Bae, Deuk-Young Nah, Namyi Gu, Hae-Young Kim
Nutr Res Pract. 2016;10(3):288-293. doi: 10.4162/nrp.2016.10.3.288.
Reference
-
1. Cook NR, Cutler JA, Obarzanek E, Buring JE, Rexrode KM, Kumanyika SK, Appel LJ, Whelton PK. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP). BMJ. 2007. 334:885–888.2. Karppanen H, Mervaala E. Sodium intake and hypertension. Prog Cardiovasc Dis. 2006. 49:59–75.3. Weinberger MH, Miller JZ, Luft FC, Grim CE, Fineberg NS. Definitions and characteristics of sodium sensitivity and blood pressure resistance. Hypertension. 1986. 8:II127–II134.4. Sullivan JM, Ratts TE. Sodium sensitivity in human subjects: hemodynamic and hormonal correlates. Hypertension. 1988. 11:717–723.5. Kawasaki T, Delea CS, Bartter FC, Smith H. The effect of high-sodium and low-sodium intakes on blood pressure and other related variables in human subjects with idiopathic hypertension. Am J Med. 1978. 64:193–198.6. Weinberger MH, Fineberg NS, Fineberg SE, Weinberger M. Salt sensitivity, pulse pressure, and death in normal and hypertensive humans. Hypertension. 2001. 37:429–432.7. O'Brien E, Sheridan J, O'Malley K. Dippers and non-dippers. Lancet. 1988. 2:397.8. Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, Matsubara M, Hashimoto J, Hoshi H, Araki T, et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens. 2002. 20:2183–2189.9. Metoki H, Ohkubo T, Kikuya M, Asayama K, Obara T, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y. Prognostic significance for stroke of a morning pressor surge and a nocturnal blood pressure decline: the Ohasama study. Hypertension. 2006. 47:149–154.10. Li Y, Thijs L, Hansen TW, Kikuya M, Boggia J, Richart T, Metoki H, Ohkubo T, Torp-Pedersen C, Kuznetsova T, et al. Prognostic value of the morning blood pressure surge in 5645 subjects from 8 populations. Hypertension. 2010. 55:1040–1048.11. Kario K, Pickering TG, Umeda Y, Hoshide S, Hoshide Y, Morinari M, Murata M, Kuroda T, Schwartz JE, Shimada K. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003. 107:1401–1406.12. Kario K, Ishikawa J, Pickering TG, Hoshide S, Eguchi K, Morinari M, Hoshide Y, Kuroda T, Shimada K. Morning hypertension: the strongest independent risk factor for stroke in elderly hypertensive patients. Hypertens Res. 2006. 29:581–587.13. Uzu T, Kazembe FS, Ishikawa K, Nakamura S, Inenaga T, Kimura G. High sodium sensitivity implicates nocturnal hypertension in essential hypertension. Hypertension. 1996. 28:139–142.14. Uzu T, Ishikawa K, Fujii T, Nakamura S, Inenaga T, Kimura G. Sodium restriction shifts circadian rhythm of blood pressure from nondipper to dipper in essential hypertension. Circulation. 1997. 96:1859–1862.15. Higashi Y, Oshima T, Ozono R, Nakano Y, Matsuura H, Kambe M, Kajiyama G. Nocturnal decline in blood pressure is attenuated by NaCl loading in salt-sensitive patients with essential hypertension: noninvasive 24-hour ambulatory blood pressure monitoring. Hypertension. 1997. 30:163–167.16. Osanai T, Okuguchi T, Kamada T, Fujiwara N, Kosugi T, Saitoh G, Katoh T, Nakano T, Takahashi K, Guan W, et al. Salt-induced exacerbation of morning surge in blood pressure in patients with essential hypertension. J Hum Hypertens. 2000. 14:57–64.17. Rhee MY, Yang SJ, Oh SW, Park Y, Kim CI, Park HK, Park SW, Park CY. Novel genetic variations associated with salt sensitivity in the Korean population. Hypertens Res. 2011. 34:606–611.18. Shin SJ, Lim CY, Rhee MY, Oh SW, Na SH, Park Y, Kim CI, Kim SY, Kim JW, Park HK. Characteristics of sodium sensitivity in Korean populations. J Korean Med Sci. 2011. 26:1061–1067.19. Staessen JA, Thijs L, Fagard R, O'Brien ET, Clement D, de Leeuw PW, Mancia G, Nachev C, Palatini P, Parati G, et al. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension: Systolic Hypertension in Europe Trial Investigators. JAMA. 1999. 282:539–546.20. Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER 3rd, Simons-Morton DG, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet: DASH-Sodium Collaborative Research Group. N Engl J Med. 2001. 344:3–10.21. Sullivan JM. Salt sensitivity: definition, conception, methodology, and long-term issues. Hypertension. 1991. 17:I61–I68.22. Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, et al. A clinical trial of the effects of dietary patterns on blood pressure: DASH Collaborative Research Group. N Engl J Med. 1997. 336:1117–1124.23. Obarzanek E, Proschan MA, Vollmer WM, Moore TJ, Sacks FM, Appel LJ, Svetkey LP, Most-Windhauser MM, Cutler JA. Individual blood pressure responses to changes in salt intake: results from the DASH-Sodium trial. Hypertension. 2003. 42:459–467.24. Gerdts E, Lund-Johansen P, Omvik P. Reproducibility of salt sensitivity testing using a dietary approach in essential hypertension. J Hum Hypertens. 1999. 13:375–384.25. Draaijer P, de Leeuw P, Maessen J, van Hooff J, Leunissen K. Salt-sensitivity testing in patients with borderline hypertension: reproducibility and potential mechanisms. J Hum Hypertens. 1995. 9:263–269.26. Weinberger MH, Fineberg NS. Sodium and volume sensitivity of blood pressure: age and pressure change over time. Hypertension. 1991. 18:67–71.27. Tuomilehto J, Jousilahti P, Rastenyte D, Moltchanov V, Tanskanen A, Pietinen P, Nissinen A. Urinary sodium excretion and cardiovascular mortality in Finland: a prospective study. Lancet. 2001. 357:848–851.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of low sodium and high potassium diet on lowering blood pressure
- Effect of a 6-month Low Sodium Diet on the Salt Taste Perception and Pleasantness, Blood Pressure and the Urinary Sodium Excretion in Female College Students
- Dietary Salt and Potassium Intake and Hypertension
- Renal Sodium Handling and Hypertension
- Salt Intake and Diabetes