J Korean Acad Periodontol.
2009 Mar;39(1):37-44. 10.5051/jkape.2009.39.1.37.
Clinical and microbiologic effects of the subantimicrobial dose of doxycycline on the chronic periodontitis
- Affiliations
-
- 1Department of Periodontology, School of Dentistry, Kangnung National University, Korea. periojk@kangnung.ac.kr
- KMID: 1783514
- DOI: http://doi.org/10.5051/jkape.2009.39.1.37
Abstract
-
PURPOSE: Tetracycline and its chemically modified non-antibacterial analogues can inhibit certain host-derived tissue destructive collagenases such as matrix metalloproteinases. The purpose of this study was to evaluate clinical and microbiologic effects of the subantimicrobial dose of doxycycline(SDD) in conjunction with scaling and root planing.
MATERIALS AND METHODS
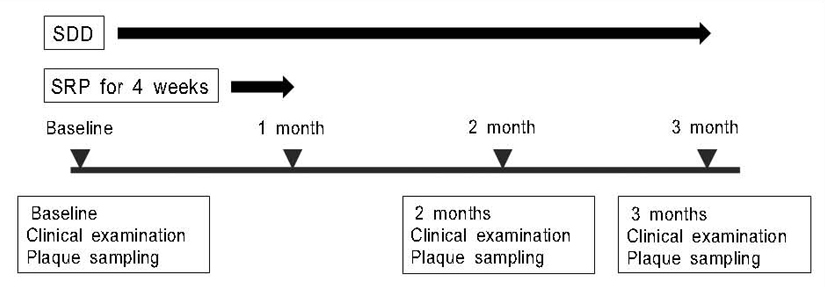
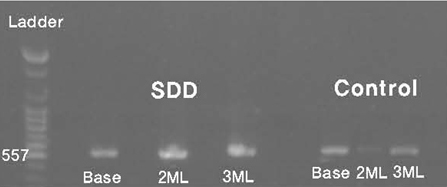
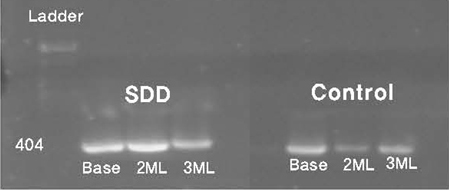
A total of 30 patients with chronic periodontitis who were going to receive scaling and root planing were randomly allocated to receive either a doxycycline hyclate for 3 months or nothing. Clinical probing depth, clinical attachment level, gingival recession, and bleeding on probing were measured by one periodontist. After a periodontal examination, microbial samples were collected using sterile paper points. The effect of SDD in conjunction with scaling and root planing on alterations of the periodontal pathogens (Aggregatibacter actinomycetemcomitans, Tannerella forsythia, Porphyromonas gingivalis) were also assessed using 16S rRNA polymerase chain reaction.
RESULTS
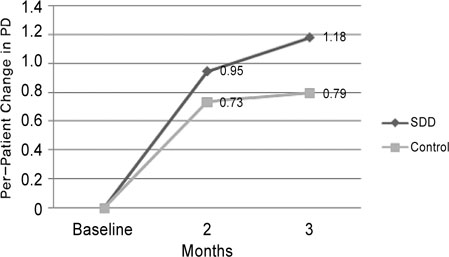
During the treatment period, clinical parameters for both treatment group and control group were improved. After 3 months, reductions in probing depth and gains in clinical attachment level were significantly greater for the SDD group than control group. Microbial analysis showed that there was no alteration of the periodontal pathogens and no difference between the groups.
CONCLUSION
This study suggested that the subantimicrobial dose of doxycycline as an adjunct therapy with scaling and root planing might be effective and safe in the management of chronic periodontitis.
MeSH Terms
Figure
Reference
-
1. Dongari-Bagtzoglou AI, Ebersole JL. Production of inflammatory mediators and cytokines by human gingival fibroblasts following bacterial challenge. J Periodontal Res. 1996. 31:90–98.
Article2. Birkedal-Hansen H, Moore WG, Bodden MK, et al. Matrix metalloproteinases: a review. Crit Rev Oral Biol Med. 1993. 4:197–250.
Article3. Birkedal-Hansen H. Role of cytokine and inflammatory mediators in tissue destruction. J Periodontal Res. 1993. 28:500–510.4. Ryan ME, Ramamurthy NS, Golub LM. Matrix metalloproteinases and their inhibition in periodontal treatment. Curr Opin Periodontol. 1996. 3:85–96.5. Newman HN. Modes of application of anti-plaque chemicals. J Clin Periodontol. 1986. 13:965–974.
Article6. Greenstein G. Local drug delivery in the treatment of periodontal diseases: Assessing the clinical significance of the results. J Periodontol. 2006. 77:565–578.
Article7. Reynolds H, Mashimo P, Slot J, et al. Use of tetracycline in the treatment of periodontitis. II. Microbiological studies. J Dent Res. 1978. 57:267.8. Slots J, Rams TE. Antibiotics in periodontal therapy: Advantages and disadvantages. J Clin Periodontol. 1990. 17:479–493.
Article9. Heijl L, Dahlen G, Sundin Y, Wenader A, Goodson JM. A 4-quadrant comparative study of periodontal treatment using tetracycline containing drug delivery fibers and scaling. J Clin Periodontol. 1991. 18:111–116.
Article10. Olsvik B, Tenover F. Tetracycline resistance in periodontal pathogens. Clin Infecta Dis. 1993. 16:Suppl. 4. 310–323.
Article11. Lee JY, Lee YM, Shin SY, et al. Effect of subantimicrobial dose doxycycline as an effective adjunct to scaling and root planing. J Periodontol. 2004. 75:1500–1508.
Article12. Golub LM, Wolff M, Lee HM, et al. Further evidence that tetracyclines inhibit collagenase activity in human crevicular fluid and from other mammalian sources. J Periodontal Res. 1985. 20:12–23.
Article13. Golub LM, Ciancio SG, Ramamurthy NS, Leung M, McNamara TF. Low-dose doxycycline therapy: effect on gingival and crevicular fluid collagenase activity in humans. J Periodontal Res. 1990. 25:321–330.
Article14. Golub LM, McNamara TF, Ryan ME. Adjunctive treatment with subantimicrobial doses of doxycycline: effects on gingival fluid collagenase activity and attachment loss in adult periodontitis. J Clin Periodontol. 2001. 28:146–156.
Article15. Golub LM, Sorsa T, Lee HM, et al. Doxycycline inhibits neutrophil(PMN)-type matrix metalloproteinases in human adult periodontitis gingiva. J Clin Periodontol. 1995. 22:100–109.
Article16. Smith GN Jr, Mickler EA, Hasty KA, Brandt KD. Specificity of inhibition of matrix metalloproteinase activity by doxycycline: relationship to structure of the enzyme. Arthritis Rheum. 1999. 42:1140–1146.
Article17. Thomas J, Walker C, Bradshaw M. Long-term use of subantimicrobial dose doxycycline does not lead to changes in antimicrobial susceptibility. J Periodontol. 2000. 71:1472–1483.
Article18. Thomas JG, Metheny RJ, Karakiozis JM, Wetzel JM, Crout RJ. Long-term sub-antimicrobial doxycycline(Periostat) as adjunctive management in adult periodontitis: effects on subgingival bacterial population dynamics. Adv Dent Res. 1998. 12:32–39.
Article19. Kim YS, Paik JW, Kim CS, Choi SH, Kim CK. Clinical effect of the subantimicrobial dose of doxycycline(SDD) on the chronic periodontitis. J Korean Acad Periodontol. 2002. 32:415–425.
Article20. Position paper. Systemic antibiotics in periodontics. J Periodontol. 2004. 75:1553–1565.21. Ashimoto A, Chen C, Bakker I, Slots J. Polymerase chain reaction detection of 8 putative periodontal pathogens in subgingival plaque of gingivitis and advanced periodontitis lesions. Oral Microbiol Immunol. 1996. 11:266–273.
Article22. Newman MG, Takei HH, Klokkevold PR, Carranza FA. Carranza's Clinical Periodontology. 2006. 10th ed. Philadelphia: W.B. Saunders;813–827.23. Howell TH, Williams RC. Nonsteroidal antiinflammatory drugs as inhibitors of periodontal disease progression. Crit Rev Oral Biol Med. 1993. 4:177–196.
Article24. Offenbacher S, Heasman PA, Collins JG. Modulation of host PGE2 secretion as a determinant of periodontal disease expression. J Periodontol. 1993. 64:Suppl. 5. 432–444.
Article25. Williams RC, Jeffcoat MK, Howell TH, et al. Three year trial of flurbiprofen treatment in humans: post-treatment period. J Dent Res. 1991. 70:468.26. Jeong SN, Han SB. The effects of low dose doxycycline regimen on gingival crevicular fluid enzyme activity of diabetic patients with periodontitis and adult periodontitis patients. J Korean Acad Periodontol. 1997. 27:701–722.
Article27. Caton JG, Ciancio SG, Blieden TM, et al. Treatment with subantimicrobial dose doxycycline improves the efficacy of scaling and root planing in patients with adult periodontitis. J Periodontol. 2000. 71:521–532.
Article28. Ciancio S, Ashley R. Safety and efficacy of sub-antimicrobial-dose doxycycline therapy in patients with adult periodontitis. Adv Dent Res. 1998. 12:27–31.
Article29. Genco RJ. Host responses in periodontal diseases: current concepts. J Periodontol. 1992. 63:Suppl. 4. 338–355.
Article30. Badersten A, Nilvéus R, Egelberg J. Effect of nonsurgical periodontal therapy. I. Moderately advanced periodontitis. J Clin Periodontol. 1981. 8:57–72.
Article31. Socransky SS, Smith C, Martin L, et al. "Checkerboard" DNA-DNA hybridization. Biotechniques. 1994. 17:788–792.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Effect of the Subantimicrobial Dose of Doxycycline(SDD) on the Chronic Periodontitis
- Clinical and microbiological investigation on the effect of doxycycline administration in the management of adult periodontitis
- The effects of low dose doxycycline regimen on gingival crevicular fluid enzyme actmty of diabetic patients with periodontitis and adult periodontitis patients
- Effect of scaling and root planing combined with systemic doxycycline therapy on glycemic control in diabetes mellitus subjects with chronic generalized periodontitis: a clinical study
- The effect of vitamin-C containing neutraceutical on periodontal wound healing as an adjunct to non-surgical or surgical periodontal treatment