Korean J Radiol.
2010 Apr;11(2):195-202. 10.3348/kjr.2010.11.2.195.
Percutaneous Intervention in Axillary Loop-Configured Arteriovenous Grafts for Chronic Hemodialysis Patients
- Affiliations
-
- 1Department of Radiology, College of Medicine, Korea University, Korea.
- 2Department of Radiology, College of Medicine, Kangwon National University, Kangwon-do 200-947, Korea. deimos@kangwon.ac.kr
- 3Department of General Thoracic and Cardiovascular Surgery, College of Medicine, Korea University, Korea.
- 4Department of Internal Medicine, College of Medicine, Korea University, Korea.
- KMID: 1783196
- DOI: http://doi.org/10.3348/kjr.2010.11.2.195
Abstract
OBJECTIVE
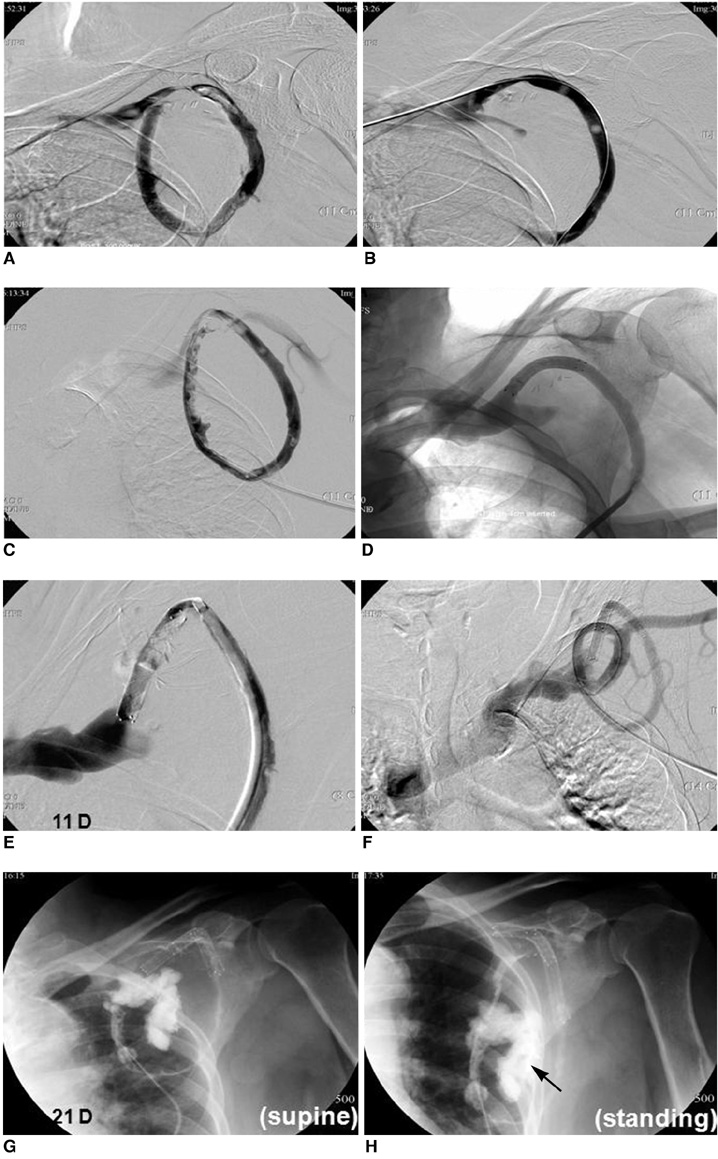
The purpose of this study was to evaluate the fistulographic features of malfunctioning axillary loop-configured arteriovenous grafts and the efficacy of percutaneous interventions in failed axillary loop-configured arteriovenous grafts.
MATERIALS AND METHODS
Ten patients with axillary loop-configured arteriovenous grafts were referred for evaluation of graft patency or upper arm swelling. Fistulography and percutaneous intervention, including thrombolysis, percutaneous transluminal angioplasty and stent placement, were performed. Statistical analysis of the procedure success rate and the primary and secondary patency rates was done.
RESULTS
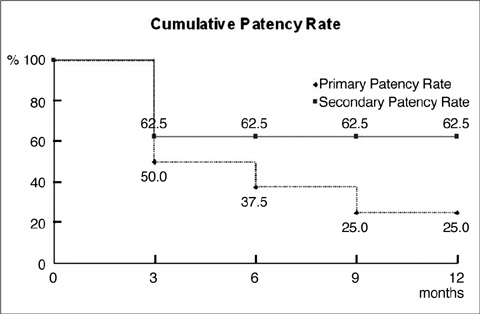
Four patients had graft related and subclavian venous stenosis, two patients had graft related stenosis and another four patients had subclavian venous stenosis only. Sixteen sessions of interventional procedures were performed in eight patients (average: 2 sessions / patient) until the end of follow-up. An interventional procedure was not done in two patients with central venous stenosis. The overall procedure success rate was 69% (11 of 16 sessions). The post-intervention primary and secondary patency rates were 50% and 63% at three months, 38% and 63% at six months and 25% and 63% at one year, respectively.
CONCLUSION
Dysfunctional axillary loop-configured arteriovenous grafts almost always had subclavian venous and graft-related stenosis. Interventional treatments are helpful to overcome this and these treatments are expected to play a major role in restoring and maintaining the axillary loop-configured arteriovenous loop grafts.
MeSH Terms
-
Adult
Aged
Angioplasty, Balloon/*methods
Arteriovenous Shunt, Surgical/*methods
Blood Vessel Prosthesis Implantation/*methods
Chronic Disease
Constriction, Pathologic/therapy/ultrasonography
Female
Follow-Up Studies
Graft Occlusion, Vascular/*therapy/ultrasonography
Humans
Kidney Failure, Chronic/*complications/therapy
Male
Middle Aged
*Renal Dialysis
Subclavian Vein/ultrasonography
Survival Analysis
Treatment Outcome
Vascular Patency
Figure
Reference
-
1. Fan PY, Schwab SJ. Vascular access: concepts for the 1990s. J Am Soc Nephrol. 1992. 3:1–11.2. Hazinedaroğlu S, Karakayali F, Tüzüner A, Ayli D, Demirer S, Duman N, et al. Exotic arteriovenous fistulas for hemodialysis. Transplant Proc. 2004. 36:59–64.3. Jean-Baptiste E, Hassen-Khodja R, Haudebourg P, Declemy S, Batt M, Bouillanne PJ. Axillary loop grafts for hemodialysis access: midterm results from a single-center study. J Vasc Surg. 2008. 47:138–143.4. Morsy MA, Khan A, Chemla ES. Prosthetic axillary-axillary arteriovenous straight access (necklace graft) for difficult hemodialysis patients: a prospective single-center experience. J Vasc Surg. 2008. 48:1251–1254.5. Teruya TH, Schaeffer D, Abou-Zamzam AM, Bianchi C. Arteriovenous graft with outflow in the proximal axillary vein. Ann Vasc Surg. 2009. 23:95–98.6. Cynamon J, Lakritz PS, Wahl SI, Bakal CW, Sprayregen S. Hemodialysis graft declotting: description of the "lyse and wait" technique. J Vasc Interv Radiol. 1997. 8:825–829.7. Hathaway PB, Vesely TM. The apex-puncture technique for mechanical thrombolysis of loop hemodialysis grafts. J Vasc Interv Radiol. 1999. 10:775–779.8. Gray RJ, Sacks D, Martin LG, Trerotola SO. Society of Interventional Radiology Technology Assessment Committee. Reporting standards for percutaneous interventions in dialysis access. J Vasc Interv Radiol. 2003. 14:S433–S442.9. Morgan AP, Knight DC, Tilney NL, Lazarus JM. Femoral triangle sepsis in dialysis patients: frequency, management, and outcome. Ann Surg. 1980. 191:460–464.10. Taylor SM, Eaves GL, Weatherford DA, McAlhany JC Jr, Russell HE, Langan EM 3rd. Results and complications of arteriovenous access dialysis grafts in the lower extremity: a five year review. Am Surg. 1996. 62:188–191.11. Blankestijin PJ. Conlon PJ, Schwab SJ, Nicholson ML, editors. Cuffed tunneled catheters for long-term vascular access. Hemodialysis vascular access practice and problems. 2001. New York: University Press;67–68.12. Manning LG, Mozersky DJ, Murray HM, Hagood CO. Axillary-axillary bovine arteriovenous fistula for hemodialysis. Arch Surg. 1975. 110:114–115.13. Duclos J, Gil F. Axillo-axillary prosthetic internal arteriovenous fistula as an alternative for vascular access in hemodialysis. Rev Med Chil. 1988. 116:49–51.14. Ono K, Muto Y, Yano K, Yukizane T. Anterior chest wall axillary artery to contralateral axillary vein graft for vascular access in hemodialysis. Artif Organs. 1995. 19:1233–1236.15. Debing E, Van den Brande P. Axillo-axillary arteriovenous fistula as a suitable surgical alternative for chronic haemodialysis access. Nephrol Dial Transplant. 1999. 4:1252–1253.16. McCann RL. Axillary grafts for difficult hemodialysis access. J Vasc Surg. 1996. 24:457–461.17. Maya ID, Oser R, Saddekni S, Barker J, Allon M. Vascular access stenosis: comparison of arteriovenous grafts and fistulas. Am J Kidney Dis. 2004. 44:859–865.18. Glanz S, Gordon DH, Lipkowitz GS, Butt KM, Hong J, Sclafani SJ. Axillary and subclavian vein stenosis: percutaneous angioplasty. Radiology. 1988. 168:371–373.19. Saeed M, Newman GE, McCann RL, Sussman SK, Braun SD, Dunnick NR. Stenoses in dialysis fistulas: treatment with percutaneous angioplasty. Radiology. 1987. 164:693–697.20. Levit RD, Cohen RM, Kwak A, Shlansky-Goldberg RD, Clark TW, Patel AA, et al. Asymptomatic central venous stenosis in hemodialysis patients. Radiology. 2006. 238:1051–1056.21. Kanterman RY, Vesely TM, Pilgram TK, Guy BW, Windus DW, Picus D. Dialysis access grafts: anatomic location of venous stenosis and results of angioplasty. Radiology. 1995. 195:135–139.22. Sreenarasimhaiah VP, Margassery SK, Martin KJ, Bander SJ. Salvage of thrombosed dialysis access grafts with venous anastomosis stents. Kidney Int. 2005. 67:678–684.23. Turmel-Rodrigues LA, Blanchard D, Pengloan J, Sapoval M, Baudin S, Testou D, et al. Wallstents and Craggstents in hemodialysis grafts and fistulas: results for selective indications. J Vasc Interv Radiol. 1997. 8:975–982.24. Zaleski GX, Funaki B, Rosenblum J, Theoharis J, Leef J. Metallic stents deployed in synthetic arteriovenous hemodialysis grafts. AJR Am J Roentgenol. 2001. 176:1515–1519.25. Patel RI, Peck SH, Cooper SG, Epstein DM, Sofocleous CT, Schur I, et al. Patency of Wallstents placed across the venous anastomosis of hemodialysis grafts after percutaneous recanalization. Radiology. 1998. 209:365–370.26. Liang HL, Pan HB, Lin YH, Chen CY, Chung HM, Wu TH, et al. Metallic stent placement in hemodialysis graft patients after insufficient balloon dilation. Korean J Radiol. 2006. 7:118–124.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intervention of the Dysfunctional and Thrombosed Autogenous Vascular Access
- Intervention Management of Arteriovenous Graft in Hemodialysis Patients
- Comparison of Clinical Outcomes in Patients Undergoing a Salvage Procedure for Thrombosed Hemodialysis Arteriovenous Grafts
- Avoiding Venous Anastomotic Dehiscence of an Arteriovenous Graft in a Super-Obese Patient
- Surgical Outcomes of Forearm Loop Arteriovenous Fistula Formation Using Tapered versus Non-Tapered Polytetrafluoroethylene Grafts