Hanyang Med Rev.
2011 Feb;31(1):38-46. 10.7599/hmr.2011.31.1.38.
Intervention of the Dysfunctional and Thrombosed Autogenous Vascular Access
- Affiliations
-
- 1Department of Radiology, Soon Chun Hyang University, Seoul Hospital, Seoul, Korea. intervention.kim@gmail.com
- KMID: 2053750
- DOI: http://doi.org/10.7599/hmr.2011.31.1.38
Abstract
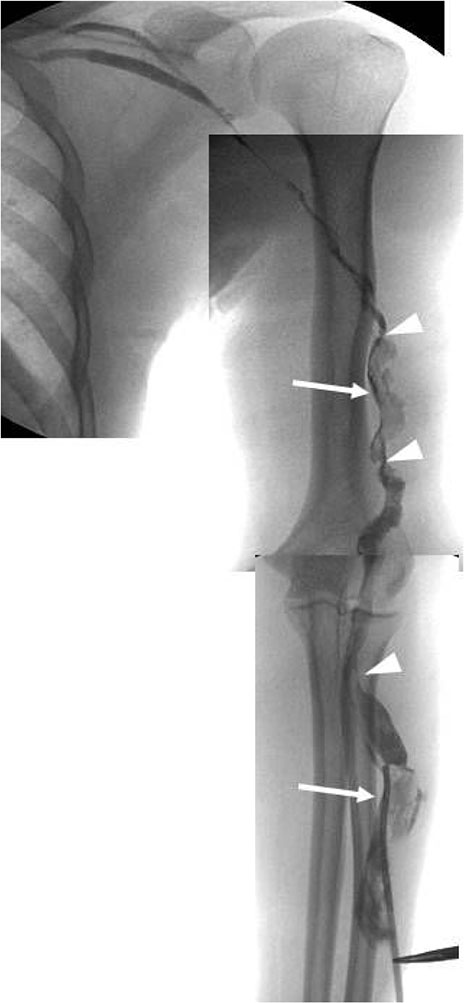
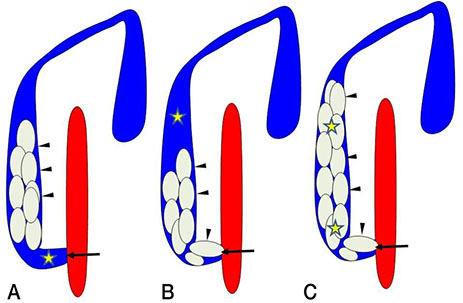
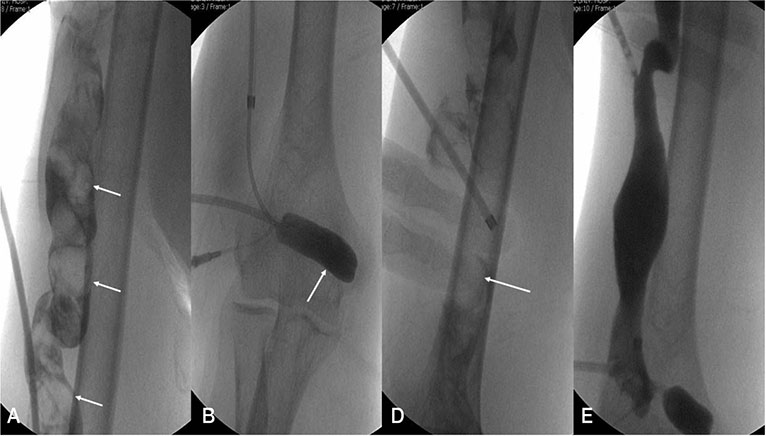
- In South Korea at the end of 2006, the total number of patients that had undergone renal replacement therapy was 46,730 (hemodialysis: 62.1%, peritoneal dialysis: 17.1%, functioning kidney transplantation: 20.8%). There were 9,197 new renal replacement therapy patients in 2006 and the incidence rate per million 185.3. In South Korea, the most common primary cause of end stage renal disease was diabetic nephropathy (42.3%), hypertensive nephrosclerosis (16.9%), and chronic glomerulonephritis (13.0%). The National Kidney Foundation Dialysis Outcomes Quality Initiative (K/DOQI) has recommended placement of autogenous arteriovenous fistulas over alternatives including the use of arteriovenous grafts and central venous catheters to improve the overall outcome of patients undergoing hemodialysis. However, autogenous arteriovenous fistulas, like polytetrafluoroethylene grafts, are also subject to dysfunction and eventual failure. Since first described in 1982, percutaneous transluminal balloon angioplasty has become the mainstay of treatment for accesses failing because of underlying central or peripheral venous stenoses. When angioplasty alone fails, alternative treatment modalities, including stent placement and atherectomy, allow immediate salvage in most cases. Consequently, interventional treatment should be attempted first for dysfunctional and thrombosed autogenous vascular access and should be initiated in all dialysis centers so long as the local radiologists are trained and enthusiastic.
Keyword
MeSH Terms
-
Angioplasty
Angioplasty, Balloon
Arteriovenous Fistula
Atherectomy
Central Venous Catheters
Constriction, Pathologic
Diabetic Nephropathies
Dialysis
Glomerulonephritis
Humans
Incidence
Kidney
Kidney Failure, Chronic
Nephrosclerosis
Polytetrafluoroethylene
Renal Dialysis
Renal Replacement Therapy
Republic of Korea
Stents
Thrombosis
Transplants
Polytetrafluoroethylene
Figure
Reference
-
1. ESRD Registry Committee of Korean Society of Nephrology. Current renal replacement therapy in Korea. Korean J Nephrol. 2006. S459–S481. (abstract book).2. Quinton W, Dillard D, Scribner BH. Cannulation of blood vessels for prolonged hemodialysis. Trans Am Soc Artif Intern Organs. 1960. 6:104–113.
Article3. Brescia MJ, Cimino JE, Appel K, Hurwich BJ. Chronic hemodialysis using venipuncture and a surgically created arteriovenous fistula. N Engl J Med. 1966. 275:1089–1092.
Article4. Chinitz JL, Yokoyama T, Bower R, Swartz C. Self-sealing prosthesis for arteriovenous fistula in man. Trans Am Soc Artif Intern Organs. 1972. 18:452–457.
Article5. NKF-DOQI clinical practice guidelines for vascular access. National Kidney Foundation-Dialysis Outcomes Quality Initiative. Am J Kidney Dis. 1997. 30:4 Suppl 3. S150–S191.6. Turmel-Rodrigues L, Pengloan J, Baudin S, Testou D, Abaza M, Dahdah G, Mouton A, Blanchard D. Treatment of stenosis and thrombosis in haemodialysis fistulas and grafts by interventional radiology. Nephrol Dial Transplant. 2000. 15:2029–2036.
Article7. Rajan DK, Bunston S, Misra S, Pinto R, Lok CE. Dysfunctional autogenous hemodialysis fistulas: outcomes after angioplasty-are there clinical predictors of patency? Radiology. 2004. 232:508–515.
Article8. Sullivan KL, Besarab A. Hemodynamic screening and early percutaneous intervention reduce hemodialysis access thrombosis and increase graft longevity. J Vasc Interv Radiol. 1997. 8:163–170.
Article9. Schwab SJ, Oliver MJ, Suhocki P, McCann R. Hemodialysis arteriovenous access: detection of stenosis and response to treatment by vascular access blood flow. Kidney Int. 2001. 59:358–362.
Article10. Beathard GA. Percutaneous transvenous angioplasty in the treatment of vascular access stenosis. Kidney Int. 1992. 42:1390–1397.
Article11. Gordon DH, Glanz S, Butt KM, Adamsons RJ, Koenig MA. Treatment of stenotic lesions in dialysis access fistulas and shunts by transluminal angioplasty. Radiology. 1982. 143:53–58.
Article12. Trerotola SO, Scheel PJ Jr, Powe NR, Prescott C, Feeley N, He J, Watson A. Screening for dialysis access graft malfunction: comparison of physical examination with US. J Vasc Interv Radiol. 1996. 7:15–20.
Article13. Rutherford RB, Becker GJ. Standards for evaluating and reporting the results of surgical and percutaneous therapy for peripheral arterial disease. JVIR. 1991. 2:169–174.
Article14. Schwab SJ, Raymond JR, Saeed M, Newman GE, Dennis PA, Bollinger RR. Prevention of hemodialysis fistula thrombosis: early detection of venous stenoses. Kidney Int. 1989. 36:707–711.
Article15. Safa AA, Valji K, Roberts AC, Ziegler TW, Hey RJ, Oglevie SB. Detection and treatment of dysfunctional hemodialysis access grafts: effect of a surveillance program on graft patency and the incidence of thrombosis. Radiology. 1996. 199:653–657.
Article16. Beathard GA. Percutaneous angioplasty for the treatment of venous stenosis: a nephrologists view. Semin Dial. 1995. 8:166–170.
Article17. Kanterman RY, Vesely TM, Pilgram TK, Guy BW, Windus DW, Picus D. Dialysis access grafts: anatomic location of venous stenosis and results of angioplasty. Radiology. 1995. 195:135–139.
Article18. Glanz S, Gordon DH, Butt KM, Hong J, Lipkowitz GS. The role of percutaneous angioplasty in the management of chronic hemodialysis fistulas. Ann Surg. 1987. 206:777–781.
Article19. Turmel-Rodrigues L, Mouton A, Birmelé B, Billaux L, Ammar N, Grezard O, Hauss S, Pengloan J. Salvage of immature forearm fistulas for hemodialysis by interventional radiology. Nephrol Dial Transplant. 2001. 16:2365–2371.20. Manninen HI, Kaukanen ET, Ikaheimo R, Karhapaa P, Lahtinen T, Matsi P, Lampainen E. Endovascular treatment of failing Brescia-Cimino hemodialysis fistulae by brachial artery access: initial success and long-term results. Radiology. 2001. 218:711–718.
Article21. Turmel-Rodrigues L, Pengloan J, Rodrigue H, Brillet G, Lataste A, Pierre D, Jourdan JL, Blanchard D. Treatment of failed native arteriovenous fistulae for hemodialysis by interventional radiology. Kidney Int. 2000. 57:1124–1140.
Article22. Haage P, Vorwerk D, Weldberger J, Piroth W, Schurmann K, Gunther RW. Percutaneous treatment of thrombosed primary arteriovenous hemodialysis access fistulae. Kidney Int. 2000. 57:1169–1175.
Article23. Turmel-Rodrigues L. Gray RJ, editor. Endovascular treatment of thrombosed autologous fistulae. Dialysis access: a multidisciplinary approach. 2002. Philadelphia: Lippincott Williams & Wilkins;229–241.24. Shatsky JB, Berns JS, Clark TW, Kwak A, Tuite CM, Shlansky-Goldberg RD, Mondschein JI, Patel AA, Stavropoulos SW, Soulen MC, Solomon JA, Kobrin S, Chittams JL, Trerotola SO. Single-center experience with the Arrow-Trerotola Percutaneous Thrombectomy Device in the management of thrombosed native dialysis fistulas. J Vasc Interv Radiol. 2005. 16:1605–1611.
Article25. Mangiarotti G, Canavese C, Thea A, Segoloni GP, Stratta P, Salomone M, Vercellone A. Urokinase treatment for arteriovenous fistulae declotting in dialyzed patients. Nephron. 1984. 36:60–64.
Article26. Poulain F, Raynaud A, Bourquelot P, Knight C, Rovani X, Gaux JC. Local thrombolysis and thromboaspiration in the treatment of acutely thrombosed arteriovenous hemodialysis fistulas. Cardiovasc Intervent Radiol. 1991. 14:98–101.
Article27. Schilling JJ, Eiser AR, Slifkin RF, Whitney JT, Neff MS. The role of thrombolysis in hemodialysis access occlusion. Am J Kidney Dis. 1987. 10:92–97.
Article28. Cohen MA, Kumpe DA, Durham JD, Zwerdlinger SC. Improved treatment of thrombosed hemodialysis access sites with thrombolysis and angioplasty. Kidney Int. 1994. 46:1375–1380.
Article29. Brunner MC, Matalon TA, Patel SK, McDonald V, Jensik SC. Ultrarapid urokinase in hemodialysis access occlusion. J Vasc Interv Radiol. 1991. 2:503–506.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hybrid surgery versus percutaneous mechanical thrombectomy for the thrombosed hemodialysis autogenous arteriovenous fistulas
- Clinical Experience with a Hybrid Procedure Using the Adherent Clot Catheter for Salvage of Thrombosed Hemodialysis Access: A Comparison with the Standard Fogarty Balloon Catheter
- Clinical Analysis of Hemodialysis Vascular Access: Comparision of Autogenous Arterioveonus Fistula & Arteriovenous Prosthetic Graft
- Efficacy of a Modified Pharmacomechanical Thrombolysis Technique for Endovascular Treatment of Thrombosed Prosthetic Arteriovenous Grafts
- Target Balloon-Assisted Antegrade and Retrograde Approach for Recanalization of Thrombosed Fem-Pop Bypass Graft Using the Outback Catheter