Korean J Radiol.
2005 Mar;6(1):22-30. 10.3348/kjr.2005.6.1.22.
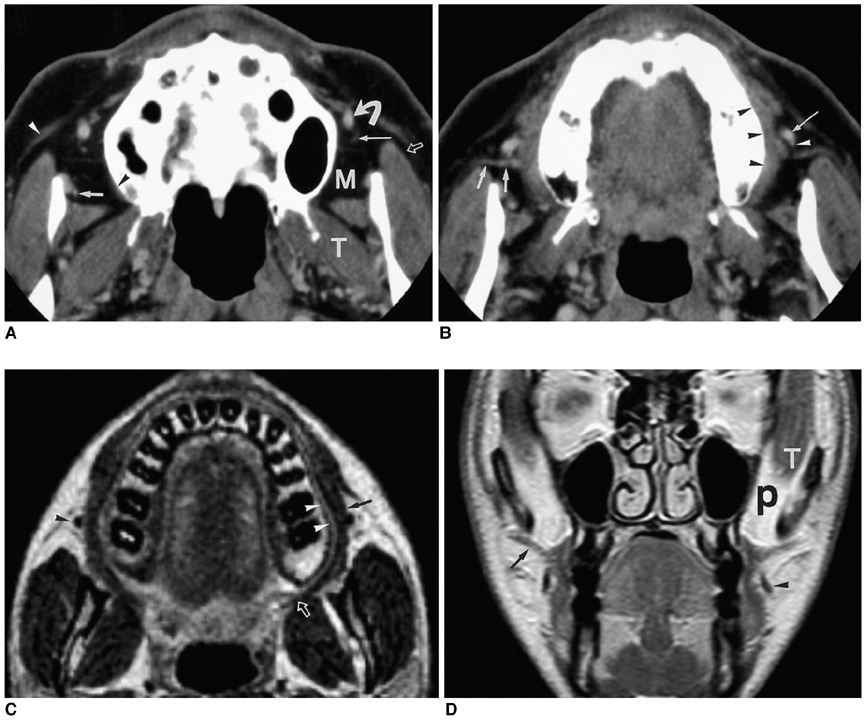
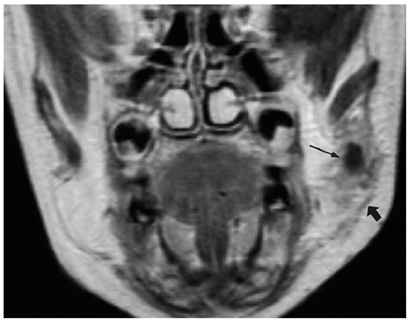
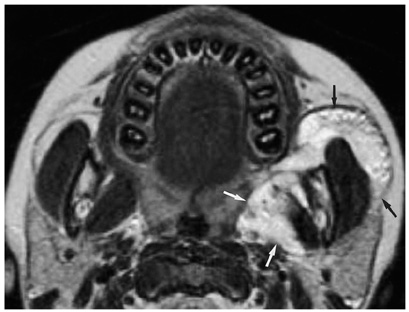
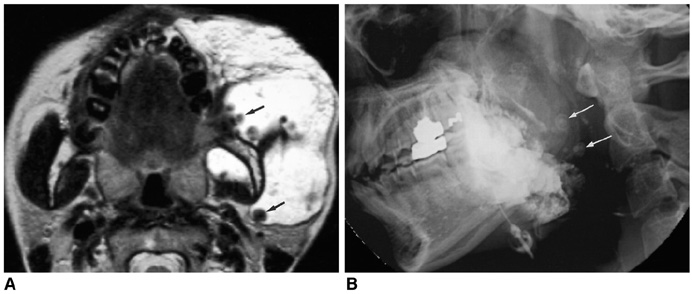
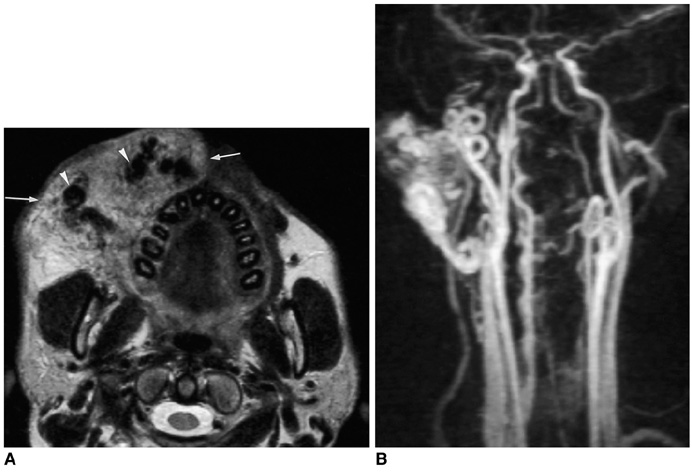
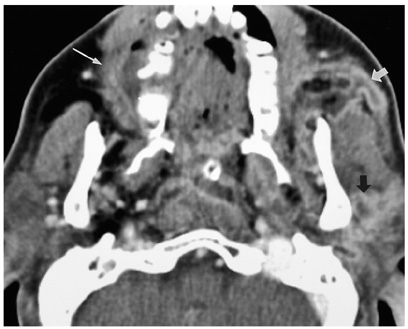
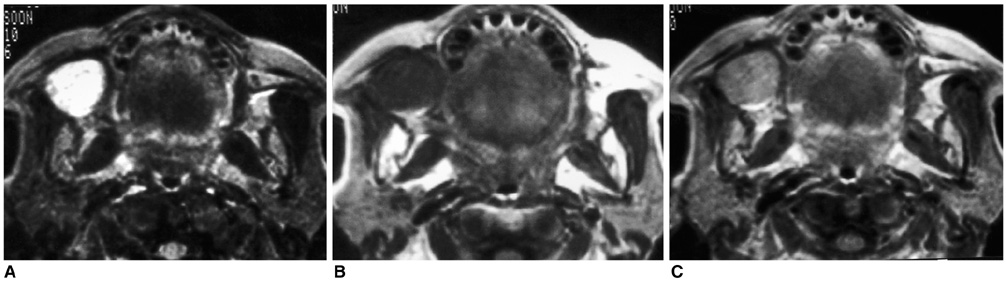
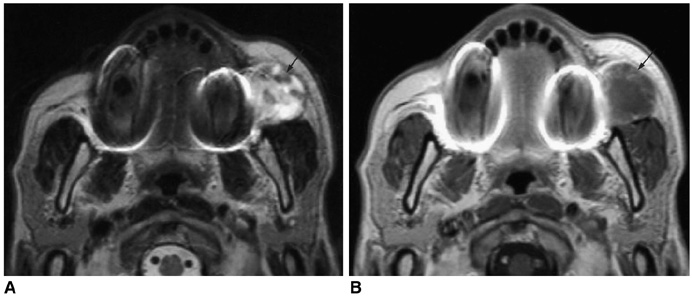
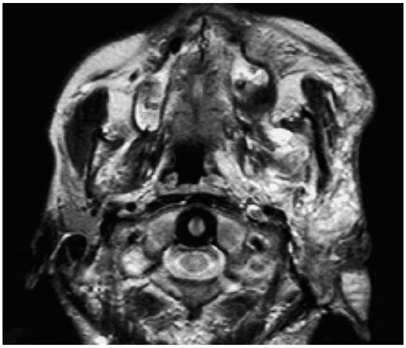
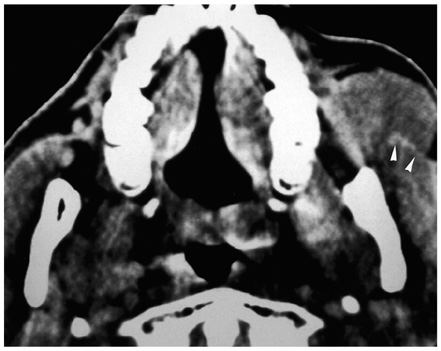
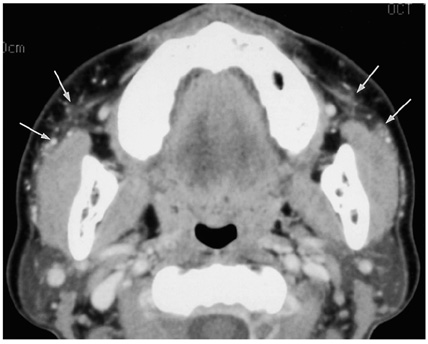
CT and MR Imaging of the Buccal Space: Normal Anatomy and Abnormalities
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine, Institute of Radiation Medicine, SNUMRC, and Clinical Research Institute, Seoul National University Hospital, Korea. hanmh@radcom.snu.ac.kr
- KMID: 1783169
- DOI: http://doi.org/10.3348/kjr.2005.6.1.22
Abstract
- The buccal space is an anatomical compartment lying anterior to the masticator space and lateral to the buccinator muscle. Since the major purpose of imaging is to define the likely anatomic origin and also the extent of a given lesion, thorough knowledge of the normal anatomy of the buccal space is essential, and this knowledge can aid the physician in narrowing down the list of possible maladies on the differential diagnosis. We illustrate here in this paper the important anatomic landmarks and typical pathologic conditions of the buccal space such as the developmental lesions and the neoplastic lesions. Knowledge of the expected pathologic conditions is useful for the radiologist when interpreting facial CT and MR images.
Keyword
MeSH Terms
Figure
Reference
-
1. Tart RP, Kotzur IM, Mancuso AA, Glantz MS, Mukherji SK. CT and MR imaging of the buccal space and buccal space masses. RadioGraphics. 1995. 15:531–550.2. Smoker WRK. Som PM, Curtin HD, editors. Oral cavity. Head and neck imaging. 1996. 3rd ed. St. Louis: Mosby;488–544.3. Kurabayashi T, Ida M, Tetsumura A, Ohbayashi N, Yasumoto M, Sasaki T. MR imaging of benign and malignant lesions in the buccal space. Dentomaxillofac Radiol. 2002. 31:344–349.4. Kurabayashi T, Ida M, Yoshino N, Sasaki T, Kishi T, Kusama M. Computed tomography in the diagnosis of buccal space masses. Dentomaxillofac Radiol. 1997. 26:347–353.5. Werner JA, Dunne AA, Folz BJ, Rochels R, Bien S, Ramaswamy A, et al. Current concepts in the classification, diagnosis and treatment of hemangiomas and vascular malformations of the head and neck. Eur Arch Otorhinolaryngol. 2001. 258:141–149.6. Baker LL, Dillon WP, Hieshima GB, Dowd CF, Frieden IJ. Hemangiomas and vascular malformations of the head and neck: MR characterization. AJNR Am J Neuroradiol. 1993. 14:307–314.7. Kern S, Niemeyer C, Darge K, Merz C, Laubenberger J, Uhl M. Differentiation of vascular birthmarks by MR imaging. An investigation of hemangiomas, venous and lymphatic malformations. Acta Radiol. 2000. 41:453–457.8. Sigal R, Monnet O, de Baere T, Micheau C, Shapeero LG, Julieron M, et al. Adenoid cystic carcinoma of the head and neck: evaluation with MR imaging and clinical-pathologic correlation in 27 patients. Radiology. 1992. 184:95–101.9. Shah GV. MR imaging of salivary glands. Magn Reson Imaging Clin N Am. 2002. 10:631–662.10. Kim HC, Han MH, Kim KH, Jae HJ, Lee SH, Kim SS, et al. Primary thyroid lymphoma: CT findings. Eur J Radiol. 2003. 46:233–239.11. Lee HJ, Im JG, Goo JM, Kim KW, Choi BI, Chang KH, et al. Peripheral T-cell lymphoma: spectrum of imaging findings with clinical and pathologic features. RadioGraphics. 2003. 23:7–26.12. Moon WK, Park JM, Kim YI, et al. Inflammatory and infectious Diseases of the breast: Imaging Findings. Postgraduate Radiol. 2000. 20:131–141.13. Som PM, Biller HF. Kimura disease involving parotid gland and cervical nodes: CT and MR findings. J Comput Assist Tomogr. 1992. 16:320–322.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of Normal Anatomy of Oral Cavity in Open-mouth View with CT and MRI: Comparison with Closed-mouth View
- Buccal Space Lesions: A New Classification Based on CT and MR Imaging Findings
- Spontaneous rupture of intrasellar cyst demonstrated by CT and MR imaging
- Inflammatory Pseudotumor of the Extraorbital Head and Neck: CT and MR Imaging Findings
- Detection of Acute Intraventricular Hemorrhage: Comparison of FLAIR MR Imaging with Unenhanced CT