Yonsei Med J.
2009 Feb;50(1):160-163. 10.3349/ymj.2009.50.1.160.
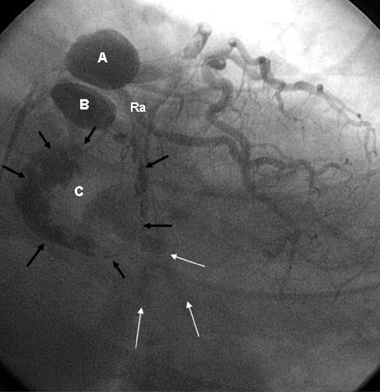
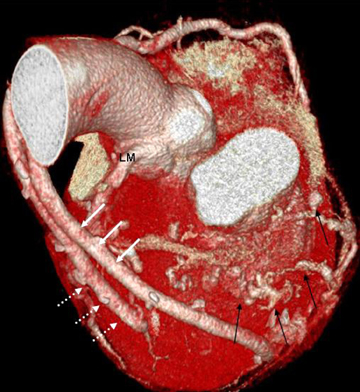
Preoperative and Postoperative Evaluation of Multiple Giant Coronary Aneurysms by the Use of Coronary CT Angiography with 64-MDCT: A Case of Multiple Giant Coronary Aneurysms Treated with Aneurysmectomy and Coronary Artery Bypass Surgery
- Affiliations
-
- 1Department of Internal Medicine, Vision 21 Cardiac and Vascular Center, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea. hmchoi49@naver.com
- 2Department of Radiology, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea.
- KMID: 1782984
- DOI: http://doi.org/10.3349/ymj.2009.50.1.160
Abstract
- A coronary artery aneurysm is an uncommon disorder and is seen as a characteristic dilatation of a localized portion of the coronary artery. Clinical manifestation of a coronary artery aneurysm varies from an asymptomatic presentation to sudden death of a patient. Although coronary aneurysms are typically diagnosed by the use of coronary angiography, a new generation of coronary 64-slice multidetector computed tomography (64-MDCT) scanners have successfully been used for evaluating this abnormality in a noninvasive manner. In the present case, we performed coronary 64-MDCT scanning preoperatively and postoperatively on a patient with multiple giant coronary aneurysms. The use of coronary 64-MDCT may provide an evaluation technique not only for diagnosis but also for follow-up after surgery for this condition.
Keyword
MeSH Terms
Figure
Reference
-
1. Swaye PS, Fisher LD, Litwin P, Vignola PA, Judkins MP, Kemp HG, et al. Aneurysmal coronary artery disease. Circulation. 1983. 67:134–138.
Article2. Ercan E, Tengiz I, Yakut N, Gurbuz A. Large atherosclerotic left main coronary aneurysm: a case report and review of literature. Int J Cardiol. 2003. 88:95–98.
Article3. Robertson T, Fisher L. Prognostic significance of coronary artery aneurysm and ectasia in the Coronary Artery Surgery Study (CASS) registry. Prog Clin Biol Res. 1987. 250:325–339.4. Wong CK, Cheng CH, Lau CP, Leung WH. Asymptomatic congenital coronary artery aneurysm in adulthood. Eur Heart J. 1989. 10:947–949.
Article5. Chia HM, Tan KH, Jackson G. Non-atherosclerotic coronary artery aneurysms: two case reports. Heart. 1997. 78:613–616.
Article6. Demopoulos VP, Olympios CD, Fakiolas CN, Pissimissis EG, Economides NM, Adamopoulou E, et al. The natural history of aneurysmal coronary artery disease. Heart. 1997. 78:136–141.
Article7. Channon KM, Banning AP, Davies CH, Bashir Y. Coronary artery aneurysm rupture mimicking dissection of the thoracic aorta. Int J Cardiol. 1998. 65:115–117.
Article8. Hinterauer L, Roelli H, Goebel N, Steinbrunn W, Senning A. Huge left coronary artery aneurysm associated with multiple arterial aneurysms. Cardiovasc Intervent Radiol. 1985. 8:127–130.
Article9. Ghanta RK, Paul S, Couper GS. Successful revascularization of multiple coronary artery aneurysms using a combination of surgical strategies. Ann Thorac Surg. 2007. 84:e10–e11.10. Westaby S, Vaccari G, Katsumata T. Direct repair of giant right coronary aneurysm. Ann Thorac Surg. 1999. 68:1401–1403.11. Peterson MA, Monsein LH, Dangas G, Mehran R, Leon MB. Percutaneous transcatheter management of giant coronary aneurysms. Circulation. 1999. 100:E8–E11.
Article12. Assiri AS. Giant coronary artery aneurysm. Ann Saudi Med. 2000. 20:248–250.
Article13. Khositeseth A, Siripornpitak S, Pornkul R, Wanitkun S. Case report: Giant coronary aneurysm caused by Kawasaki disease: follow-up with echocardiography and multidetector CT angiography. Br J Radiol. 2008. 81:e106–e109.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple Giant Coronary Aneurysms Arising from Coronary Fistula to the Pulmonary Artery Revealed in Aorta CT Angiography
- Right Coronary Artery to Left Ventricular Fistula with a Giant Right Coronary Artery Aneurysm: A case report
- Two Cases of Super-Giant Coronary Aneurysms after Kawasaki Disease
- CABG for Treating Unstable Angina with Multivessel Coronary Artery Aneurysms: A case report
- The Noninvasive Diagnosis and Postoperative Evaluation of Anomalous Right Coronary Artery from the Pulmonary Artery (ARCAPA) using Coronary MDCT: A Case Report