Korean J Radiol.
2006 Jun;7(2):118-124. 10.3348/kjr.2006.7.2.118.
Metallic Stent Placement in Hemodialysis Graft Patients after Insufficient Balloon Dilation
- Affiliations
-
- 1Department of Radiology, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan. cfyang@isca.vghks.gov.tw
- 2National Yang-Ming University, Taipei, Taiwan.
- 3Department of Internal Medicine, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan.
- 4Department of Vascular Surgery, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan.
- 5Fooyin University, Kaohsiung Hsien, Taiwan.
- KMID: 1782184
- DOI: http://doi.org/10.3348/kjr.2006.7.2.118
Abstract
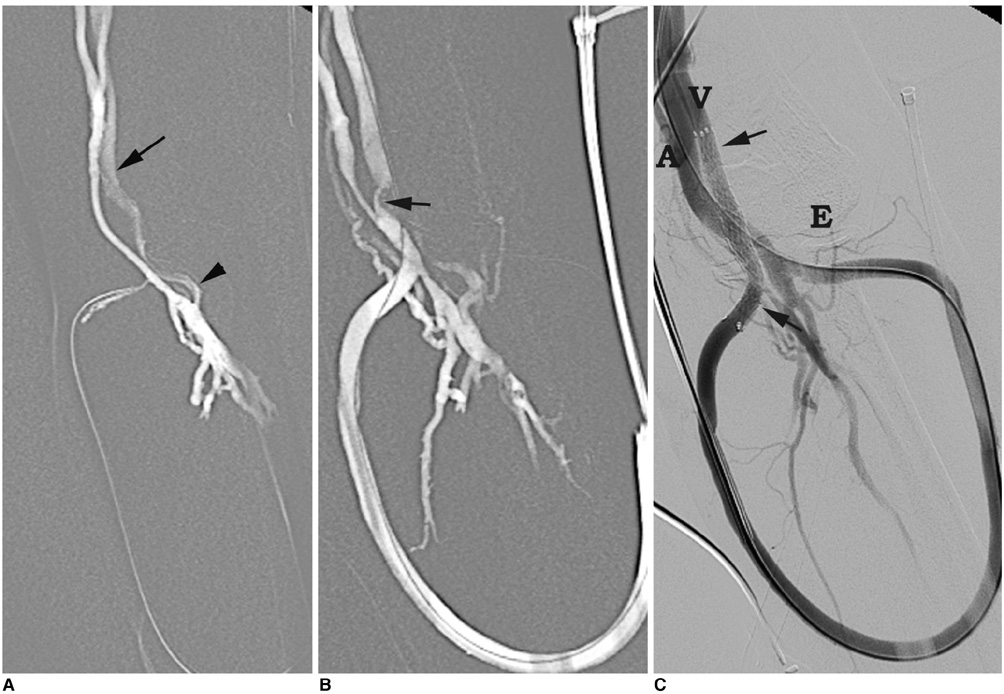
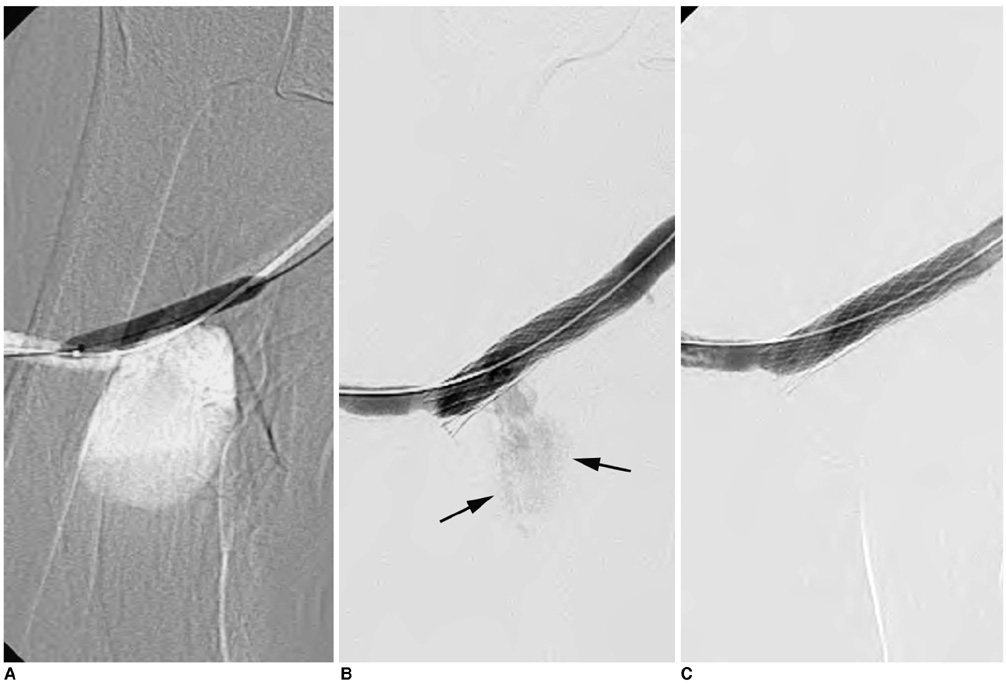
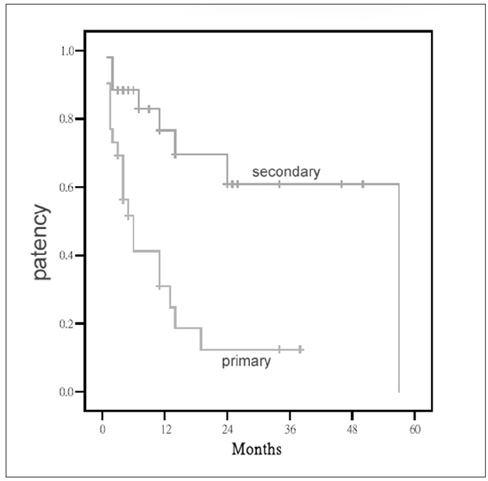
OBJECTIVE
We wanted to report our experience of metallic stent placement after insufficient balloon dilation in graft hemodialysis patients. MATERIALS AND METHODS: Twenty-three patients (13 loop grafts in the forearm and 10 straight grafts in the upper arm) underwent metallic stent placement due to insufficient flow after urokinase thrombolysis and balloon dilation. The indications for metallic stent deployment included 1) recoil and/or kinked venous stenosis in 21 patients (venous anastomosis: 17 patients, peripheral outflow vein: four patients); and 2) major vascular rupture in two patients. Metallic stents 8-10mm in diameter and 40-80 mm in length were used. Of them, eight stents were deployed across the elbow crease. Access patency was determined by clinical follow-up and the overall rates were calculated by Kaplan-Meier survival analysis. RESULTS: No procedure-related complications (stent fracture or central migration) were encountered except for a delayed Wallstent shortening/migration at the venous anastomosis, which resulted in early access failure. The overall primary and secondary patency rates (+/- standard error) of all the vascular accesses in our 23 patients at 3, 6, 12 and 24 months were 69% +/- 9 and 88% +/- 6, 41% +/- 10 and 88% +/- 6, 30% +/- 10 and 77% +/- 10, and 12% +/- 8 and 61% +/- 13, respectively. For the forearm and upper-arm grafts, the primary and secondary patency rates were 51% +/- 16 and 86% +/- 13 vs 45% +/- 15 and 73%+/-13 at 6 months, and 25% +/- 15 and 71% +/- 17 vs 23% +/- 17 and 73% +/- 13 at 12 months (p = .346 and .224), respectively. CONCLUSION: Metallic stent placement is a safe and effective means for treating peripheral venous lesions in dialysis graft patients after insufficient balloon dilation. No statistically difference in the patency rates between the forearm and upper-arm patient groups was seen.
MeSH Terms
Figure
Reference
-
1. Beathard GA. Percutaneous transvenous angioplasty in the treatment of vascular access stenosis. Kidney Int. 1992. 42:1390–1397.2. Valji K, Bookstein JJ, Roberts AC, Oglevie SB, Pittman C, O'Neill MP. Pulse-spray pharmacomechanical thrombolysis of thrombosed hemodialysis access grafts: long-term experience and comparison of original and current techniques. AJR Am J Roentgenol. 1995. 164:1495–1500.3. Gray RJ. Percutaneous intervention for permanent hemodialysis access: a review. J Vasc Interv Radiol. 1997. 8:313–327.4. Turmel-Rodrigues L, Pengloan J, Bourquelot P. Interventional radiology in hemodialysis fistulae and grafts: a multidisciplinary approach. Cardiovasc Intervent Radiol. 2002. 25:3–16.5. Quinn SF, Schuman ES, Demlow TA, Standage BA, Ragsdale JW, Green GS, et al. Percutaneous transluminal angioplasty versus endovascular stent placement in the treatment of venous stenoses in patients undergoing hemodialysis: intermediate results. J Vasc Interv Radiol. 1995. 6:851–855.6. Hoffer EK, Sultan S, Herskowitz MM, Daniels ID, Sclafani SJ. Prospective randomized trial of a metallic intravascular stent in hemodialysis graft maintenance. J Vasc Interv Radiol. 1997. 8:965–973.7. Vorwerk D, Guenther RW, Mann H, Bohndorf K, Keulers P, Alzen G, et al. Venous stenosis and occlusion in hemodialysis shunts: follow-up results of stent placement in 65 patients. Radiology. 1995. 195:140–146.8. Funaki B, Szymski GX, Leef JA, Funaki AN, Lorenz J, Farrell T, et al. Treatment of venous outflow stenoses in thigh grafts with Wallstents. AJR Am J Roentgenol. 1999. 172:1591–1596.9. Patel RI, Peck SH, Cooper SG, Epstein DM, Sofocleous CT, Schur I, et al. Patency of Wallstents placed across the venous anastomosis of hemodialysis grafts after percutaneous recanalization. Radiology. 1998. 209:365–370.10. Raynaud AC, Angel CY, Sapoval MR, Beyssen B, Pagny JY, Auguste M. Treatment of hemodialysis access rupture during PTA with Wallstent implantation. J Vasc Interv Radiol. 1998. 9:437–442.11. Welber A, Schur I, Sofocleous CT, Cooper SG, Patel RI, Peck SH. Endovascular stent placement for angioplasty-induced venous rupture related to the treatment of hemodialysis grafts. J Vasc Interv Radiol. 1999. 10:547–551.12. Funaki B, Szymski GX, Leef JA, Rosenblum JD, Burke R, Hackworth CA. Wallstent deployment to salvage dialysis graft thrombolysis complicated by venous rupture: early and intermediate results. AJR Am J Roentgenol. 1997. 169:1435–1437.13. Clark TW. Nitinol stents in hemodialysis access. J Vasc Interv Radiol. 2004. 15:1037–1040.14. Kolakowski S Jr, Dougherty MJ, Calligaro KD. Salvaging prosthetic dialysis fistulas with stents: forearm versus upper arm grafts. J Vasc Surg. 2003. 38:719–723.15. Vogel PM, Parise C. SMART stent for salvage of hemodialysis access grafts. J Vasc Interv Radiol. 2004. 15:1051–1060.16. Turmel-Rodrigues L, Pengloan J, Blanchier D, Abaza M, Birmele B, Haillot O, et al. Insufficient dialysis shunts: improved long-term patency rates with close hemodynamic monitoring, repeated percutaneous balloon angioplasty, and stent placement. Radiology. 1993. 187:273–278.17. Palder SB, Kirkman RL, Whittemore AD, Hakim RM, Lazarus JM, Tilney NL. Vascular access for hemodialysis: patency rates and results for revision. Ann Surg. 1985. 202:235–239.18. Sapoval MR, Turmel-Rodrigues LA, Raynaud AC, Bourquelot P, Rodrigue H, Gaux JC. Cragg covered stents in hemodialysis access: initial and midterm results. J Vasc Interv Radiol. 1996. 7:335–342.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Malignant Strictures Involving the Esophagogastric Junction: Palliative Treatment with Balloon Dilation Combined with Chemotherapy and/or Radiotherapy
- Stent Flange-Induced Esophageal Stricture Treated with an Oral Steroid
- Comparison of Helical Interwoven Nitinol Stent Placement Versus Balloon Angioplasty for Arteriovenous Dialysis Graft Malfunction Caused by Stenosis of the Venous Anastomosis Site
- Expandable Metallic Stent Placement for Nutcracker Syndrome
- Self-Expandable Metallic Stent Therapy for a Gastrointestinal Benign Stricture