J Korean Med Sci.
2011 Feb;26(2):297-300. 10.3346/jkms.2011.26.2.297.
Catheter-related Candidemia Caused by Candida haemulonii in a Patient in Long-term Hospital Care
- Affiliations
-
- 1Division of Infectious Disease, Department of Internal Medicine, Kyung Hee University College of Medicine, Seoul, Korea. sonjs@korea.com
- 2Asia Pacific Foundation for Infectious Diseases (APFID), Seoul, Korea.
- 3Department of Molecular Cell Biology, Sungkyunkwan University School of Medicine, Suwon, Korea.
- KMID: 1782122
- DOI: http://doi.org/10.3346/jkms.2011.26.2.297
Abstract
- Candida haemulonii, one of the non-albicans Candida species, is an emerging yeast pathogen that is known to be resistant to amphotericin B and other antifungal agents such as azoles. These anti-fungal agents have often been associated with clinical treatment failure, so no treatment regimen has been clearly established for invasive C. haemulonii infections. We investigated a catheter-related infection of C. haemulonii candidemia in an adult patient in long-term hospital care. In the early stages, the candidemia remained persistent despite treatment with fluconazole. However, after changing the antifungal agent to caspofungin, the candidemia was resolved. Fluconazole and amphotericin B are not reliable empirical antifungal agents for invasive C. haemulonii infections, as shown in previous case reports. An echinocandin such as caspofungin may be an appropriate empirical choice of antifungal agent for an invasive C. haemulonii infection.
Keyword
MeSH Terms
-
Aged
Amphotericin B/therapeutic use
Antifungal Agents/therapeutic use
Candida/classification/isolation & purification/*pathogenicity
Candidiasis/drug therapy/*microbiology
Catheter-Related Infections/drug therapy/*microbiology
Echinocandins/therapeutic use
Fluconazole/therapeutic use
*Hospitals
Humans
*Long-Term Care
Male
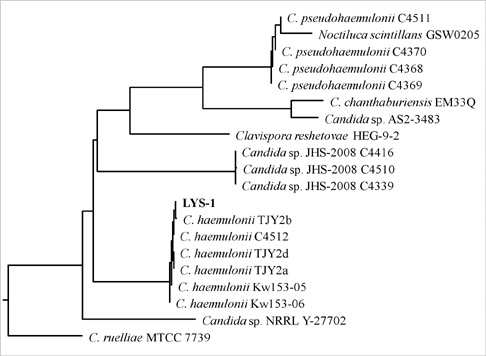
Phylogeny
Figure
Reference
-
1. Pfaller MA, Diekema DJ. International Fungal Surveillance Participant Group. Twelve years of fluconazole in clinical practice: global trends in species distribution and fluconazole susceptibility of bloodstream isolates of Candida. Clin Microbiol Infect. 2004. 10:Suppl 1. 11–23.2. Vazquez JA, Lundstrom T, Dembry L, Chandrasekar P, Boikov D, Parri MB, Zervos MJ. Invasive Candida guilliermondii infection: in vitro susceptibility studies and molecular analysis. Bone Marrow Transplant. 1995. 16:849–853.3. Gargeya IB, Pruitt WR, Meyer SA, Ahearn DG. Candida haemulonii from clinical specimens in the USA. J Med Vet Mycol. 1991. 29:335–338.4. García-Martos P, Domínguez I, Marín P, García-Agudo R, Aoufi S, Mira J. Antifungal susceptibility of emerging yeast pathogens. Enferm Infecc Microbiol Clin. 2001. 19:249–256.5. Khan ZU, Al-Sweih NA, Ahmad S, Al-Kazemi N, Khan S, Joseph L, Chandy R. Outbreak of fungemia among neonates caused by Candida haemulonii resistant to amphotericin B, itraconazole, and fluconazole. J Clin Microbiol. 2007. 45:2025–2027.6. Ruan SY, Kuo YW, Huang CT, Hsiue HC, Hsueh PR. Infections due to Candida haemulonii: species identification, antifungal susceptibility and outcomes. Int J Antimicrob Agents. 2010. 35:85–88.7. Van Uden N, Kolipinski MC. Torulopsis haemulonii nov spec a yeast from the Atlantic Ocean. Antonie Van Leeuwenhoek. 1962. 28:78–80.8. Lavarde V, Daniel F, Saez H, Arnold M, Faguer B. Peritonite mycosique a Torulopsis haemulonii. Bull Soc Fr Mycol Med. 1984. 13:173–176.9. Rodero L, Cuenca-Estrella M, Córdoba S, Cahn P, Davel G, Kaufman S, Guelfand L, Rodríguez-Tudela JL. Transient fungemia caused by an amphotericin B-resistant isolate of Candida haemulonii. J Clin Microbiol. 2002. 40:2266–2269.10. Kim MN, Shin JH, Sung H, Lee K, Kim EC, Ryoo N, Lee JS, Jung SI, Park KH, Kee SJ, Kim SH, Shin MG, Suh SP, Ryang DW. Candida haemulonii and closely related species at 5 university hospitals in Korea: identification, antifungal susceptibility, and clinical features. Clin Infect Dis. 2009. 48:e57–e61.11. Hong SK, Nam SH, Kim HC. Fatal peripheral candidal suppurative thrombophlebitis in a postoperative patient. J Korean Med Sci. 2008. 23:1094–1096.12. Han SS, Yim JJ, Yoo CG, Kim YW, Han SK, Shim YS, Lee SM. Clinical characteristics and risk factors for nosocomial candidemia in medical intensive care units: experience in a single hospital in Korea for 6.6 years. J Korean Med Sci. 2010. 25:671–676.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Prospective Study of Intraocular Candidiasis
- Clinical and Laboratory Features of Candidemia Caused by Different Candida Species
- Clinical Significance of Pastorex Candida Antigen Assay in Patients with Candidemia
- Risk Factors for the Development of Nosocomial Candidemia among Patients in Intensive Care Unit
- Risk Factors and Prognosis for Persistent Candidemia without Catheter Colonization