Yonsei Med J.
2010 Nov;51(6):870-876. 10.3349/ymj.2010.51.6.870.
Assessment of Deceased Donor Kidneys Using a Donor Scoring System
- Affiliations
-
- 1Department of Internal Medicine, Eulji University School of Medicine, Daejeon, Korea.
- 2Department of Medicine, Sungkyunkwan University School of Medicine, Suwon, Korea.
- 3Department of Internal Medicine, University of Ulsan College of Medicine, Seoul, Korea.
- 4Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. curie@snu.ac.kr
- 5Department of Surgery, Seoul National University College of Medicine, Seoul, Korea.
- 6Department of Laboratory Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 7Department of Surgery, Sungkyunkwan University School of Medicine, Suwon, Korea.
- 8Transplantation Center, Seoul National University Hospital, Seoul, Korea. jcyjs@dreamwiz.com
- 9Transplantation Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 10Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 1779633
- DOI: http://doi.org/10.3349/ymj.2010.51.6.870
Abstract
- PURPOSE
Marginal grafts should be used more actively in Asian countries where deceased donor transplantation is unpopular. We modified a quantitative donor scoring system proposed by Nyberg and his colleagues and developed a donor scoring system in order to assess the quality of deceased donor grafts and their prognostic value as an initial effort to promote usage of marginal donors.
MATERIALS AND METHODS
We retrospectively evaluated 337 patients.
RESULTS
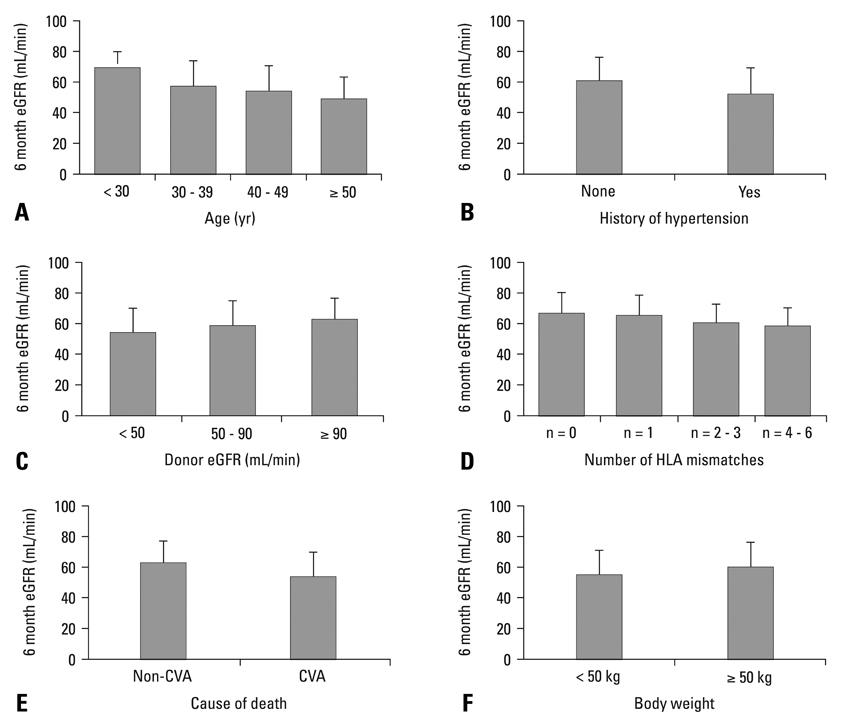
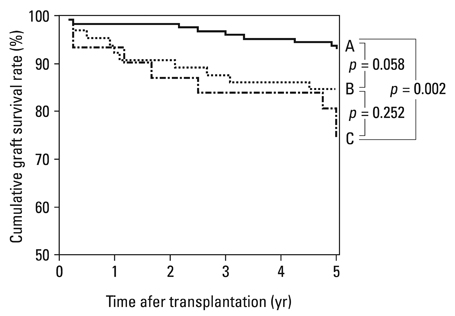
A scoring system was derived from six donor variables [age, 0-25; renal function, 0-4; history of hypertension, 0-4; Human Leukocyte Antigen (HLA) mismatch, 0-3; body weight, 0-1; cause of death, 0-3 points]. Donor grafts were stratified by scores: grade A, 0-10; grade B, 11-20; grade C, 21-30; and grade D, 31-40 points. Donor grades significantly correlated with estimated glomerular filtration rate (eGFR) at 6 months (A, 64.0 mL/min/1.73 m2; B, 57.0 mL/min/1.73 m2; C, 46.8 mL/min/1.73 m2; p < 0.001). The five-year graft survival rate was also lower in grade C than grade A (74% vs. 93%, p = 0.002). Donors in grade C and D were regarded as marginal donors. The proportion of marginal donors was much lower in Korea, compared with data from the United Network for Organ Sharing (15.2% vs. 29%).
CONCLUSION
Considering the scarcity of deceased donor kidneys and the relatively better graft outcome with lower grade-donors in Korea, it is worth increasing the usage of marginal grafts.
Keyword
MeSH Terms
Figure
Reference
-
1. International Registry Organ Donation and Transplantation. http://www.tpm.org.2. Miranda B, Gonzalez Alvarez I, Cuende N, Naya MT, De Felipe C. Update on organ donation and retrieval in Spain. Nephrol Dial Transplant. 1999. 14:842–845.
Article3. Port FK, Bragg-Gresham JL, Metzger RA, Dykstra DM, Gillespie BW, Young EW, et al. Donor characteristics associated with reduced graft survival: an approach to expanding the pool of kidney donors. Transplantation. 2002. 74:1281–1286.
Article4. Metzger RA, Delmonico FL, Feng S, Port FK, Wynn JJ, Merion RM. Expanded criteria donors for kidney transplantation. Am J Transplant. 2003. 3:Suppl 4. 114–125.
Article5. Nyberg SL, Baskin-Bey ES, Kremers W, Prieto M, Henry ML, Stegall MD. Improving the prediction of donor kidney quality: deceased donor score and resistive indices. Transplantation. 2005. 80:925–929.
Article6. Nyberg SL, Matas AJ, Kremers WK, Thostenson JD, Larson TS, Prieto M, et al. Improved scoring system to assess adult donors for cadaver renal transplantation. Am J Transplant. 2003. 3:715–721.
Article7. Nyberg SL, Matas AJ, Rogers M, Harmsen WS, Velosa JA, Larson TS, et al. Donor scoring system for cadaveric renal transplantation. Am J Transplant. 2001. 1:162–170.
Article8. Levey AS, Greene T, Kusek J, Beck GJ, Group MS. A simplified equation to predict glomerular filtration rate from serum creatinine [Abstract]. J Am Soc Nephrol. 2000. 11:A0828.9. Cho YW, Terasaki PI, Cecka JM, Gjertson DW, Takemoto S. Should excessive height and weight differences between the kidney donor and recipient be avoided? Transplant Proc. 1997. 29:104–105.
Article10. Kasiske BL, Snyder JJ, Gilbertson D. Inadequate donor size in cadaver kidney transplantation. J Am Soc Nephrol. 2002. 13:2152–2159.
Article11. Nyengaard JR, Bendtsen TF. Glomerular number and size in relation to age, kidney weight, and body surface in normal man. Anat Rec. 1992. 232:194–201.
Article12. Kasiske BL, Umen AJ. The influence of age, sex, race, and body habitus on kidney weight in humans. Arch Pathol Lab Med. 1986. 110:55–60.
Article13. White AJ, Strydom WJ. Normalisation of glomerular filtration rate measurements. Eur J Nucl Med. 1991. 18:385–390.
Article14. Newman EV, Bordley J, Winternitz J. The interrelationships of glomerular filtration rate (mannitol clearance), extracellular fluid volume, surface area of the body, and plasma concentration of mannitol. Johns Hopkins Med J. 1944. 75:253–268.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation and Utilization of Expanded Criteria Dornor
- Primary non-function in a deceased donor kidney transplant even with a Kidney Donor Risk Index less than 1.0: a case report
- Study for the Relationship between the Post-Transplant Renal Function and the Donor Score Using Deceased Donor Scoring System
- Liver retransplantation for adult recipients
- Validation of the KDRI in Korean Deceased Donor Kidney Transplantation