Disseminated Hemangioblastomatosis of the Central Nervous System without von Hippel-Lindau Disease: A Case Report
- Affiliations
-
- 1Department of Neurosurgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jilee@skku.edu
- 2Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Diagnostic and Laboratory Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1779217
- DOI: http://doi.org/10.3346/jkms.2009.24.4.755
Abstract
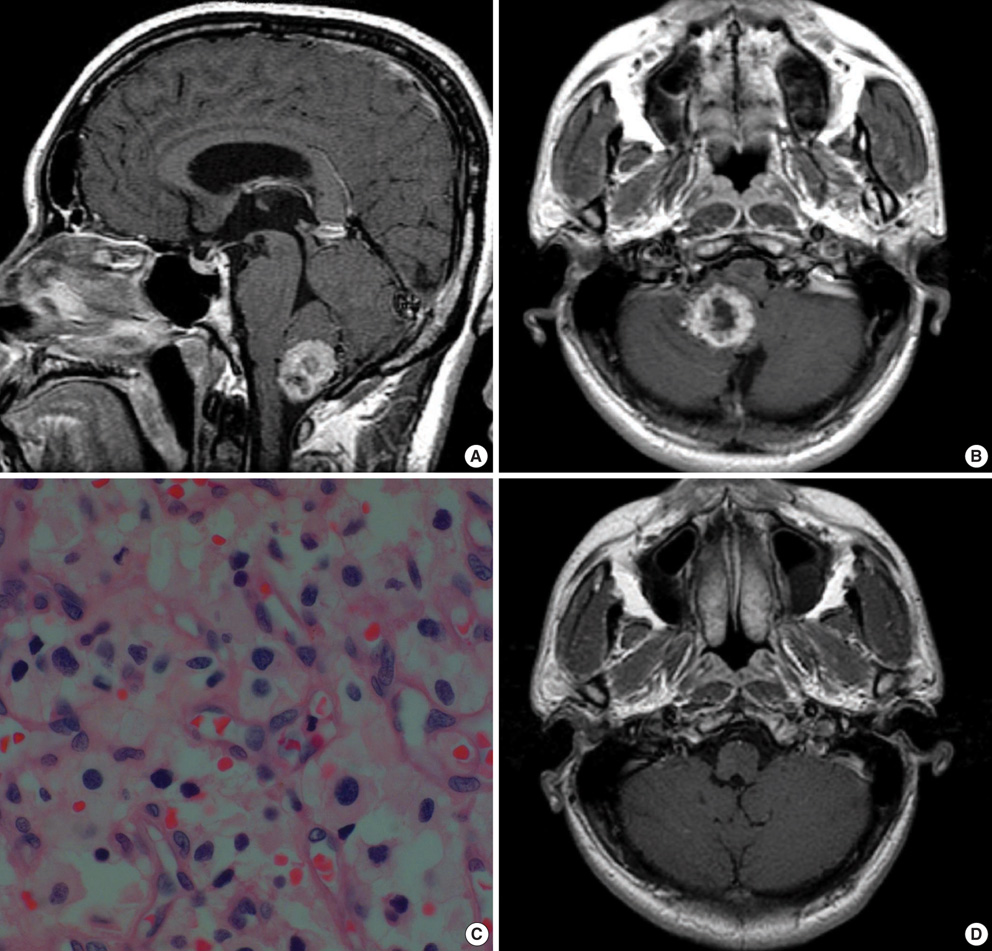
- We report a very rare case of hemangioblastomatosis that developed after surgical removal of a solitary cerebellar hemangioblastoma (HB). A 51-yr-old man presented with back pain 10 yr after undergoing surgery for cerebellar HB. Magnetic resonance imaging showed numerous mass lesions along the entire neuraxis accompanied by prominent leptomeningeal enhancement. Genomic DNA analysis showed no mutation in the von Hippel-Lindau (VHL) genes. A surgical specimen obtained from a lesion in the cauda equina showed pathological findings identical to those of the cerebellar HB that had been resected 10 yr earlier. External beam radiation therapy and radiosurgery were subsequently performed; however, the patient succumbed one year after receiving the diagnosis of hemangioblastomatosis. The reduction of tumor cell spillage during surgery and regular long-term follow-up are recommended for patients with HBs.
MeSH Terms
Figure
Cited by 3 articles
-
Disseminated Hemangioblastoma of the Central Nervous System without Von Hippel-Lindau Disease
Sun-Yoon Chung, Sin-Soo Jeun, Jae-Hyun Park
Brain Tumor Res Treat. 2014;2(2):96-101. doi: 10.14791/btrt.2014.2.2.96.Pituitary Stalk Hemangioblastoma in a von Hippel-Lindau Patient : Clinical Course Follow-Up Over a 20-Year Period
Kyung Mi Lee, Eui Jong Kim, Woo Suk Choi, Tae Sung Kim
J Korean Neurosurg Soc. 2013;53(5):297-299. doi: 10.3340/jkns.2013.53.5.297.Central Nervous System Dissemination of Solitary Sporadic Supratentorial Hemangioblastoma: A Case Report and Literature Review
Seong-Chan Jung, In-Young Kim, Shin Jung, Tae-Young Jung, Kyung-Sub Moon, Yeong-Jin Kim, Sue-Jee Park, Kyung-Hwa Lee
Brain Tumor Res Treat. 2024;12(1):80-86. doi: 10.14791/btrt.2023.0047.
Reference
-
1. Choyke PL, Filling-Katz MR, Shawker TH, Gorin MB, Travis WD, Chang R, Seizinger BR, Dwyer AJ, Linehan WM. von Hippel-Lindau disease: radiologic screening for visceral manifestations. Radiology. 1990. 174:815–820.
Article2. Choyke PL, Glenn GM, Walther MM, Patronas NJ, Linehan WM, Zbar B. von Hippel-Lindau disease: genetic, clinical, and imaging features. Radiology. 1995. 194:629–642.
Article3. Eisenhofer G, Lenders JW, Linehan WM, Walther MM, Goldstein DS, Keiser HR. Plasma normetanephrine and metanephrine for detecting pheochromocytoma in von Hippel-Lindau disease and multiple endocrine neoplasia type 2. N Engl J Med. 1999. 340:1872–1879.
Article4. Glasker S, Bender BU, Apel TW, van Velthoven V, Mulligan LM, Zentner J, Neumann HP. Reconsideration of biallelic inactivation of the VHL tumour suppressor gene in hemangioblastomas of the central nervous system. J Neurol Neurosurg Psychiatry. 2001. 70:644–648.
Article5. Neumann HP, Eggert HR, Weigel K, Friedburg H, Wiestler OD, Schollmeyer P. Hemangioblastomas of the central nervous system. A 10-year study with special reference to von Hippel-Lindau syndrome. J Neurosurg. 1989. 70:24–30.6. Singounas EG. Haemangioblastomas of the central nervous system. Acta Neurochir (Wien). 1978. 44:107–113.
Article7. Lee JY, Dong SM, Park WS, Yoo NJ, Kim CS, Jang JJ, Chi JG, Zbar B, Lubensky IA, Linehan WM, Vortmeyer AO, Zhuang Z. Loss of heterozygosity and somatic mutations of the VHL tumor suppressor gene in sporadic cerebellar hemangioblastomas. Cancer Res. 1998. 58:504–508.8. Richard S, David P, Marsot-Dupuch K, Giraud S, Beroud C, Resche F. Central nervous system hemangioblastomas, endolymphatic sac tumors, and von Hippel-Lindau disease. Neurosurg Rev. 2000. 23:1–22.
Article9. Niemela M, Lemeta S, Summanen P, Bohling T, Sainio M, Kere J, Poussa K, Sankila R, Haapasalo H, Kaariainen H, Pukkala E, Jaaskelainen J. Long-term prognosis of haemangioblastoma of the CNS: impact of von Hippel-Lindau disease. Acta Neurochir (Wien). 1999. 141:1147–1156.10. Bakshi R, Mechtler LL, Patel MJ, Lindsay BD, Messinger S, Gibbons KJ. Spinal leptomeningeal hemangioblastomatosis in von Hippel-Lindau disease: magnetic resonance and pathological findings. J Neuroimaging. 1997. 7:242–244.
Article11. Mohan J, Brownell B, Oppenheimer DR. Malignant spread of haemangioblastoma: report on two cases. J Neurol Neurosurg Psychiatry. 1976. 39:515–525.
Article12. Reyns N, Assaker R, Louis E, Lejeune JP. Leptomeningeal hemangioblastomatosis in a case of von Hippel-Lindau disease: case report. Neurosurgery. 2003. 52:1212–1215.
Article13. Tohyama T, Kubo O, Kusano R, Miura N, Himuro H. A case of hemangioblastoma with subarachnoid dissemination. No Shinkei Geka. 1990. 18:83–88.14. Weil RJ, Vortmeyer AO, Zhuang Z, Pack SD, Theodore N, Erickson RK, Oldfield EH. Clinical and molecular analysis of disseminated hemangioblastomatosis of the central nervous system in patients without von Hippel-Lindau disease. Report of four cases. J Neurosurg. 2002. 96:775–787.15. Kato M, Ohe N, Okumura A, Shinoda J, Nomura A, Shuin T, Sakai N. Hemangioblastomatosis of the central nervous system without von Hippel-Lindau disease: a case report. J Neurooncol. 2005. 72:267–270.
Article16. Hanse MC, Vincent A, van den Bent MJ. Hemangioblastomatosis in a patient with von Hippel-Lindau disease. J Neurooncol. 2007. 82:163–164.
Article17. Hammel PR, Vilgrain V, Terris B, Penfornis A, Sauvanet A, Correas JM, Chauveau D, Balian A, Beigelman C, O'Toole D, Bernades P, Ruszniewski P, Richard S. Pancreatic involvement in von Hippel-Lindau disease. The Groupe Francophone d'Etude de la Maladie de von Hippel-Lindau. Gastroenterology. 2000. 119:1087–1095.18. Hough DM, Stephens DH, Johnson CD, Binkovitz LA. Pancreatic lesions in von Hippel-Lindau disease: prevalence, clinical significance, and CT findings. AJR Am J Roentgenol. 1994. 162:1091–1094.
Article19. Lonser RR, Glenn GM, Walther M, Chew EY, Libutti SK, Linehan WM, Oldfield EH. von Hippel-Lindau disease. Lancet. 2003. 361:2059–2067.
Article20. Girmens JF, Erginay A, Massin P, Scigalla P, Gaudric A, Richard S. Treatment of von Hippel-Lindau retinal hemangioblastoma by the vascular endothelial growth factor receptor inhibitor SU5416 is more effective for associated macular edema than for hemangioblastomas. Am J Ophthalmol. 2003. 136:194–196.
Article21. Niemela M, Maenpaa H, Salven P, Summanen P, Poussa K, Laatikainen L, Jaaskelainen J, Joensuu H. Interferon alpha-2a therapy in 18 hemangioblastomas. Clin Cancer Res. 2001. 7:510–516.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multifocal Spinal Hemangioblastoma in von Hippel-Lindau Syndrome: A Case Report and Literature Review
- Von Hippel-Lindau disease: A Case Report
- Familial Occurrence of Von hippel-Lindau Disease: Case Report
- Pancreatic Cyst in von Hippel-Lindau Disease
- Three Cases of Cerebellar Hemangioblastoma in a von Hippel-Lindau Family: Case Report