J Korean Surg Soc.
2009 Oct;77(4):287-290. 10.4174/jkss.2009.77.4.287.
Pancreatic Cyst in von Hippel-Lindau Disease
- Affiliations
-
- 1Department of Surgery, Holy Family Hospital, The Catholic University of Korea, Bucheon, Korea. parkiy@catholic.ac.kr
- KMID: 1464889
- DOI: http://doi.org/10.4174/jkss.2009.77.4.287
Abstract
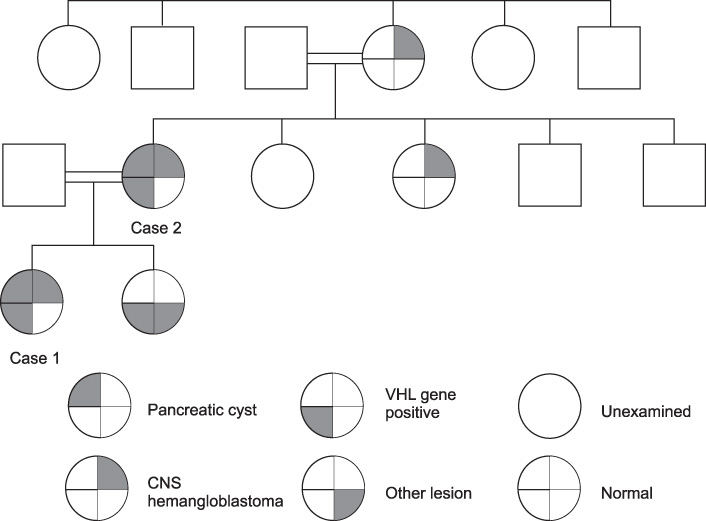
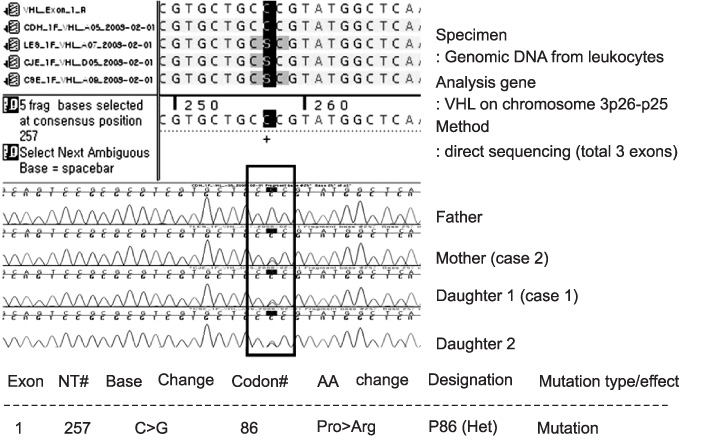
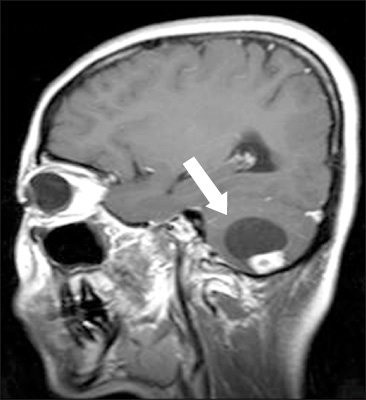
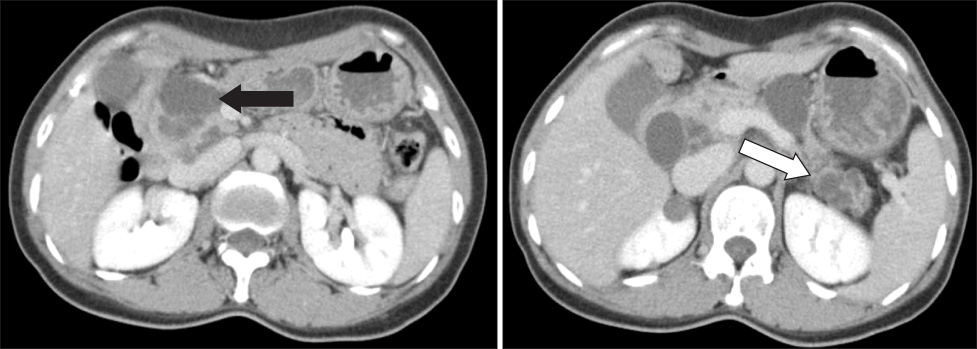
- The von Hippel-Lindau (VHL) disease is an autosomal dominant disorder by germline mutation of VHL tumor suppressor gene. The affected patients mainly develop cancers of the central nervous system, renal cell carcinoma, pheochromocytoma, and pancreatic cysts. Pancreatic involvement was observed 12~77% in VHL patients and included true cysts, serous cystadenomas, and neuroendocrine tumors. We experienced two cases of pancreatic cyst of the von Hippel-Lindau disease and reviewed associated literatures.
Keyword
MeSH Terms
Figure
Reference
-
1. Lamiell JM, Salazar FG, Hsia YE. von Hippel-Lindau disease affecting 43 members of a single kindred. Medicine (Baltimore). 1989. 68:1–29.2. Hough DM, Stephens DH, Johnson CD, Binkovitz LA. Pancreatic lesions in von Hippel-Lindau disease: prevalence, clinical significance, and CT findings. AJR Am J Roentgenol. 1994. 162:1091–1094.3. Hammel PR, Vilgrain V, Terris B, Penfornis A, Sauvanet A, Correas JM, et al. Pancreatic involvement in von Hippel-Lindau disease. The Groupe Francophone d'Etude de la Maladie de von Hippel-Lindau. Gastroenterology. 2000. 119:1087–1095.4. Perez-Ordonez B, Naseem A, Lieberman PH, Klimstra DS. Solid serous adenoma of the pancreas. The solid variant of serous cystadenoma? Am J Surg Pathol. 1996. 20:1401–1405.5. Libutti SK, Choyke PL, Bartlett DL, Vargas H, Walther M, Lubensky I, et al. Pancreatic neuroendocrine tumors associated with von Hippel Lindau disease: diagnostic and management recommendations. Surgery. 1998. 124:1153–1159.6. Neumann HP, Wiestler OD. Clustering of features and genetics of von Hippel-Lindau syndrome. Lancet. 1991. 338:258.7. Chen F, Kishida T, Yao M, Hustad T, Glavac D, Dean M, et al. Germline mutations in the von Hippel-Lindau disease tumor suppressor gene: correlations with phenotype. Hum Mutat. 1995. 5:66–75.8. Maher ER, Yates JR, Harries R, Benjamin C, Harris R, Moore AT, et al. Clinical features and natural history of von Hippel-Lindau disease. Q J Med. 1990. 77:1151–1163.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Von Hippel-Lindau Disease Diagnosed by Initial Symptoms of Urologic Manifestation
- Papillary Cystadenoma of the Epididymis: Component of von Hippel-Lindau Syndrome: A case report
- Von Hippel-Lindau disease: A Case Report
- Two Cases of Multiple Hemangioblastomas in a Von Hippel-Lindau Family
- Familial Occurrence of Von hippel-Lindau Disease: Case Report