J Korean Med Sci.
2011 Apr;26(4):507-512. 10.3346/jkms.2011.26.4.507.
Clinical Significance of a Large Difference (> or = 2 points) between Biopsy and Post-prostatectomy Pathological Gleason Scores in Patients with Prostate Cancer
- Affiliations
-
- 1Department of Urology, College of Medicine, Hallym University, Chuncheon, Korea.
- 2Department of Urology, Asan Medical Center, University of Ulsan, College of Medicine, Seoul, Korea.
- 3Department of Urology, Sungkyunkwan University, School of Medicine, Seoul, Korea. hanyong.choi@samsung.com
- 4Department of Urology, Seoul St. Mary's Hospital, College of Medicine, The Catholic university of Korea, Seoul, Korea.
- 5Department of Urology, College of Medicine, Korea University, Seoul, Korea.
- 6Urologic Oncology Clinic, National Cancer Center, Goyang, Korea.
- 7Department of Urology, College of Medicine, Kyungpook National University, Daegu, Korea.
- 8Department of Urology, Seoul Veterans Hospital, Seoul, Korea.
- 9Department of Urology, College of Medicine, Pusan National University, Busan, Korea.
- 10Department of Urology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 11Department of Urology, Seoul National University, College of Medicine, Seoul, Korea.
- 12Department of Urology, Urological Science Institute, Yonsei University, College of Medicine, Seoul, Korea.
- 13Department of Urology, Chonbuk National University Medical School, Jeonju, Korea.
- 14Department of Urology, College of Medicine, Chungbuk National University, Cheongju, Korea.
- KMID: 1777880
- DOI: http://doi.org/10.3346/jkms.2011.26.4.507
Abstract
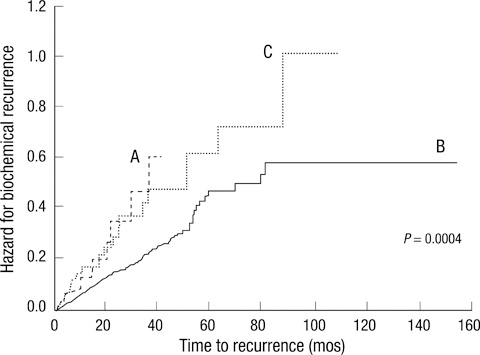
- We investigated the clinical significance of large difference (> or = 2 points) between biopsy-derived (bGS) and post-prostatectomy Gleason scores (pGS). At 14 medical centers in Korea, 1,582 men who underwent radical prostatectomy for prostate cancer were included. According to the difference between bGS and pGS, the patients were divided into three groups: A (decreased in pGS > or = 2, n = 30), B (changed in pGS < or = 1, n = 1,361; control group), and C (increased in pGS > or = 2, n = 55). We evaluated various clinicopathological factors of prostate cancer and hazards for biochemical failure. Group A showed significantly higher mean maximal percentage of cancer in the positive cores (max%) and pathological T stage than control. In group C, the number of biopsy core was significantly smaller, however, tumor volume and max% were significantly higher and more positive biopsy cores were presented than control. Worse pathological stage and more margin-positive were observed in group A and C than in control. Hazard ratio for biochemical failure was also higher in group A and C (P = 0.001). However, the groups were not independent factors in multivariate analysis. In conclusion, large difference between bGS and pGS shows poor prognosis even in the decreased group. However it is not an independent prognostic factor for biochemical failure.
Keyword
MeSH Terms
Figure
Reference
-
1. Edwards BK, Brown ML, Wingo PA, Howe HL, Ward E, Ries LA, Schrag D, Jamison PM, Jemal A, Wu XC, Friedman C, Harlan L, Warren J, Anderson RN, Pickle LW. Annual report to the nation on the status of cancer, 1975-2002, featuring population-based trends in cancer treatment. J Natl Cancer Inst. 2005. 97:1407–1427.2. Jung KW, Park S, Kong HJ, Won YJ, Boo YK, Shin HR, Park EC, Lee JS. Cancer statistics in Korea: incidence, mortality and survival in 2006-2007. J Korean Med Sci. 2010. 25:1113–1121.3. Gleason DF, Mellinger GT. Prediction of prognosis for prostatic adenocarcinoma by combined histological grading and clinical staging. J Urol. 1974. 111:58–64.4. Lerner SE, Blute ML, Bergstralh EJ, Bostwick DG, Eickholt JT, Zincke H. Analysis of risk factors for progression in patients with pathologically confined prostate cancers after radical retropubic prostatectomy. J Urol. 1996. 156:137–143.5. Epstein JI, Partin AW, Sauvageot J, Walsh PC. Prediction of progression following radical prostatectomy. A multivariate analysis of 721 men with long-term follow-up. Am J Surg Pathol. 1996. 20:286–292.6. Smith EB, Frierson HF Jr, Mills SE, Boyd JC, Theodorescu D. Gleason scores of prostate biopsy and radical prostatectomy specimens over the past 10 years: is there evidence for systematic upgrading? Cancer. 2002. 94:2282–2287.7. Moussa AS, Li J, Soriano M, Klein EA, Dong F, Jones JS. Prostate biopsy clinical and pathological variables that predict significant grading changes in patients with intermediate and high grade prostate cancer. BJU Int. 2009. 103:43–48.8. Epstein JI, Allsbrook WC Jr, Amin MB, Egevad LL. ISUP Grading Committee. The 2005 International Society of Urological Pathology (ISUP) Consensus Conference of Gleason grading of prostatic carcinoma. Am J Surg Pathol. 2005. 29:1228–1242.9. Köksal IT, Ozcan F, Kadioglu TC, Esen T, Kiliçaslan I, Tunç M. Discrepancy between Gleason scores of biopsy and radical prostatectomy specimens. Eur Urol. 2000. 37:670–674.10. Catalona WJ, Stein AJ, Fair WR. Grading errors in prostatic needle biopsies: relation to the accuracy of tumor grade in predicting pelvic lymph node metastases. J Urol. 1982. 127:919–922.11. Müller HA, Ackermann R, Frohmüller HG. The value of perineal punch biopsy in estimating the histological grade of carcinoma of the prostate. Prostate. 1980. 1:303–309.12. Aihara M, Wheeler TM, Ohori M, Scardino PT. Heterogeneity of prostate cancer in radical prostatectomy specimens. Urology. 1994. 43:60–66.13. Ruijter ET, van de Kaa CA, Schalken JA, Debruyne FM, Ruiter DJ. Histological grade heterogeneity in multifocal prostate cancer. Biological and clinical implications. J Pathol. 1996. 180:295–299.14. Harnden P, Shelley MD, Coles B, Staffurth J, Mason MD. Should the Gleason grading system for prostate cancer be modified to account for high-grade tertiary components? A systematic review and meta-analysis. Lancet Oncol. 2007. 8:411–419.15. Mosse CA, Magi-Galluzzi C, Tsuzuki T, Epstein JI. The prognostic significance of tertiary Gleason pattern 5 in radical prostatectomy specimens. Am J Surg Pathol. 2004. 28:394–398.16. van Oort IM, Schout BM, Kiemeney LA, Hulsbergen CA, Witjes JA. Does the tertiary Gleason pattern influence the PSA progression-free interval after retropubic radical prostatectomy for organ confined prostate cancer? Eur Urol. 2005. 48:572–576.17. Capitanio U, Karakiewicz PI, Valiquette L, Perrotte P, Jeldres C, Briganti A, Gallina A, Suardi N, Cestari A, Guazzoni G, Salonia A, Montorsi F. Biopsy core number represents one of foremost predictors of clinically significant Gleason sum upgrading in patients with low-risk prostate cancer. Urology. 2009. 73:1087–1091.18. Turley RS, Terris MK, Kane CJ, Aronson WJ, Presti JC Jr, Amling CL, Freedland SJ. SEARCH Database Study Group. The association between prostate size and Gleason score upgrading depends on the number of biopsy cores obtained: results from the Shared Equal Access Regional Cancer Hospital Database. BJU Int. 2008. 102:1074–1079.19. Allsbrook WC Jr, Mangold KA, Johnson MH, Lane RB, Lane CG, Epstein JI. Interobserver reproducibility of Gleason grading of prostatic carcinoma: general pathologist. Hum Pathol. 2001. 32:81–88.20. McLean M, Srigley J, Banerjee D, Warde P, Hao Y. Interobserver variation in prostate cancer Gleason scoring: are there implications for the design of clinical trials and treatment strategies? Clin Oncol (R Coll Radiol). 1997. 9:222–225.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Use of Serum PSA in Comparison of Biopsy Gleason Score with Radical Prostatectomy Gleason Score
- The Evaluation of Concordance of the Gleason Score between Prostatectomy and Biopsies Showing more than Two Different Gleason Scores in Positive Cores
- Incidence of Pathological Downgrading and Treatment Outcome After Radical Prostatectomy in Patients With Biopsy Confirmed High Gleason Score Prostate Cancer
- Predictors of Gleason Score Upgrading after Radical Prostatectomy in Low-Risk Prostate Cancer
- Clinical Significance of Calculated Prostate Cancer Volume as the Predictor of Pathologic Stage