J Korean Med Sci.
2011 May;26(5):599-603. 10.3346/jkms.2011.26.5.599.
Long-term Mortality in Adult Orthotopic Heart Transplant Recipients
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Asan Medical Center, College of Medicine, University of Ulsan, Seoul, Korea. jwlee@amc.seoul.kr
- 2Department of Cardiology, Asan Medical Center, College of Medicine, University of Ulsan, Seoul, Korea.
- KMID: 1777856
- DOI: http://doi.org/10.3346/jkms.2011.26.5.599
Abstract
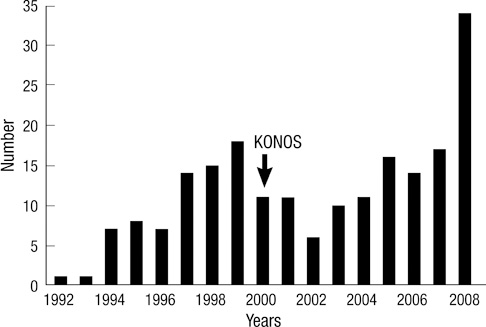
- Heart transplantation is now regarded as the treatment of choice for end-stage heart failure. To improve long-term results of the heart transplantation, we analyzed causes of death relative to time after transplantation. A total of 201 consecutive patients, 154 (76.6%) males, aged > or = 17 yr underwent heart transplantation between November 1992 and December 2008. Mean ages of recipients and donors were 42.8 +/- 12.4 and 29.8 +/- 9.6 yr, respectively. The bicaval anastomosis technique was used since 1999. Mean follow up duration was 6.5 +/- 4.4 yr. Two patients (1%) died in-hospital due to sepsis caused by infection. Late death occurred in 39 patients (19.4%) with the most common cause being sepsis due to infection. The 1-, 5-, and 10-yr survival rates in these patients were 95.5% +/- 1.5%, 86.9% +/- 2.6%, and 73.5% +/- 4.1%, respectively. The surgical results of heart transplantation in adults were excellent, with late mortality due primarily to infection, malignancy, and rejection. Cardiac deaths related to cardiac allograft vasculopathy were very rare.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Current Status of Heart Transplantation and Left Ventricular Assist Device: Major Changes in the Last Decade
Sook Jin Lee, Suk Geun Hong
Hanyang Med Rev. 2014;34(4):185-196. doi: 10.7599/hmr.2014.34.4.185.Acute Myocardial Infarction due to Cardiac Allograft Vasculopathy: An Autopsy Report
Moon-Young Kim, Jang Han Kim, Min Jee Park, Soong Deok Lee
Korean J Leg Med. 2018;42(3):92-97. doi: 10.7580/kjlm.2018.42.3.92.
Reference
-
1. Fonarow GC, Abraham WT, Albert NM, Stough WG, Gheorghiade M, Greenberg BH, O'Connor CM, Sun JL, Yancy C, Young JB. OPTIMIZE-HF Investigators and Hospitals. Age- and gender-related differences in quality of care and outcomes of patients hospitalized with heart failure (from OPTIMIZE-HF). Am J Cardiol. 2009. 104:107–115.2. Kalogeropoulos A, Georgiopoulou V, Kritchevsky SB, Psaty BM, Smith NL, Newman AB, Rodondi N, Satterfield S, Bauer DC, Bibbins-Domingo K, Smith AL, Wilson PW, Vasan RS, Harris TB, Butler J. Epidemiology of incident heart failure in a contemporary elderly cohort: the health, aging, and body composition study. Arch Intern Med. 2009. 169:708–715.3. Hunt SA, Haddad F. The changing face of heart transplantation. J Am Coll Cardiol. 2008. 52:587–598.4. Taylor DO, Edwards LB, Aurora P, Christie JD, Dobbels F, Kirk R, Rahmel AO, Kucheryavaya AY, Hertz MI. Registry of the International Society for Heart and Lung Transplantation: twenty-fifth official adult heart transplant report--2008. J Heart Lung Transplant. 2008. 27:943–956.5. Lower RR, Stofer RC, Shumway NE. Homovital transplantation of the heart. J Thorac Cardiovasc Surg. 1961. 41:196–204.6. Choo SJ, Kim JJ, Kim SP, Lee JW, Wan RS, Park NH, Lee SK, Yoo DG, Song H, Chung CH, Kim KS, Song MG. Heart transplantation. A retrospective analysis of the long-term results. Yonsei Med J. 2004. 45:1173–1180.7. Sarsam MA, Campbell CS, Yonan NA, Deiraniya AK, Rahman AN. An alternative surgical technique in orthotopic cardiac transplantation. J Card Surg. 1993. 8:344–349.8. el Gamel A, Yonan NA, Grant S, Deiraniya AK, Rahman AN, Sarsam MA, Campbell CS. Orthotopic cardiac transplantation: a comparison of standard and bicaval Wythenshawe techniques. J Thorac Cardiovasc Surg. 1995. 109:721–729.9. Luckraz H, Goddard M, Charman SC, Wallwork J, Parameshwar J, Large SR. Early mortality after cardiac transplantation: should we do better? J Heart Lung Transplant. 2005. 24:401–405.10. Taylor DO, Stehlik J, Edwards LB, Aurora P, Christie JD, Dobbels F, Kirk R, Kucheryavaya AY, Rahmel AO, Hertz MI. Registry of the International Society for Heart and Lung Transplantation: Twenty-sixth Official Adult Heart Transplant Report-2009. J Heart Lung Transplant. 2009. 28:1007–1022.11. Leyh RG, Jahnke AW, Kraatz EG, Sievers HH. Cardiovascular dynamics and dimensions after bicaval and standard cardiac transplantation. Ann Thorac Surg. 1995. 59:1495–1500.12. Traversi E, Pozzoli M, Grande A, Forni G, Assandri J, Viganò M, Tavazzi L. The bicaval anastomosis technique for orthotopic heart transplantation yields better atrial function than the standard technique: an echocardiographic automatic boundary detection study. J Heart Lung Transplant. 1998. 17:1065–1074.13. Meyer SR, Modry DL, Bainey K, Koshal A, Mullen JC, Rebeyka IM, Ross DB, Bowker S, Wang S. Declining need for permanent pacemaker insertion with the bicaval technique of orthotopic heart transplantation. Can J Cardiol. 2005. 21:159–163.14. Park KY, Park CH, Chun YB, Shin MS, Lee KC. Bicaval anastomosis reduces tricuspid regurgitation after heart transplantation. Asian Cardiovasc Thorac Ann. 2005. 13:251–254.15. Aziz T, Burgess M, Khafagy R, Wynn Hann A, Campbell C, Rahman A, Deiraniya A, Yonan N. Bicaval and standard techniques in orthotopic heart transplantation: medium-term experience in cardiac performance and survival. J Thorac Cardiovasc Surg. 1999. 118:115–122.16. Weiss ES, Nwakanma LU, Russell SB, Conte JV, Shah AS. Outcomes in bicaval versus biatrial techniques in heart transplantation: an analysis of the UNOS database. J Heart Lung Transplant. 2008. 27:178–183.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- CMV Disease
- Outcomes of liver transplant recipients in 5 years postoperative period
- Lived Experiences of Korean Young Adults After Heart Transplantation: A Phenomenological Approach
- Malignancy in Renal Transplant Recipients
- The impact of early tacrolimus exposure to long-term renal function and growth in pediatric liver transplant recipients