Korean J Radiol.
2000 Mar;1(1):5-10. 10.3348/kjr.2000.1.1.5.
Primary Antiphospholipid Antibody Syndrome: Neuro radiologic Findings in 11 Patients
- Affiliations
-
- 1Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 1777289
- DOI: http://doi.org/10.3348/kjr.2000.1.1.5
Abstract
OBJECTIVE
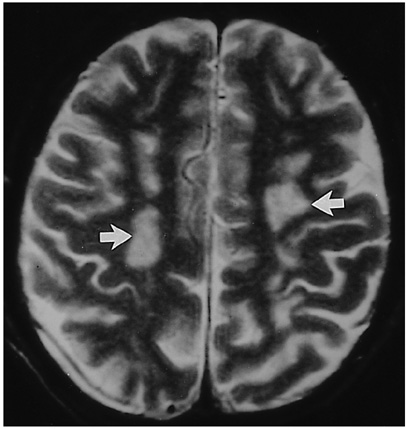
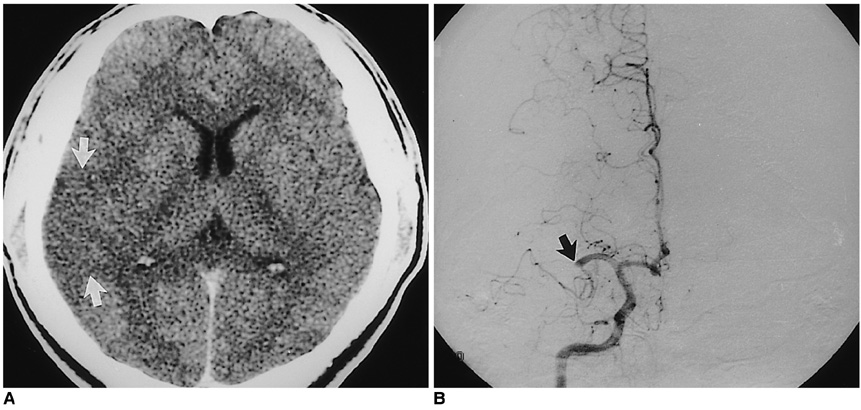
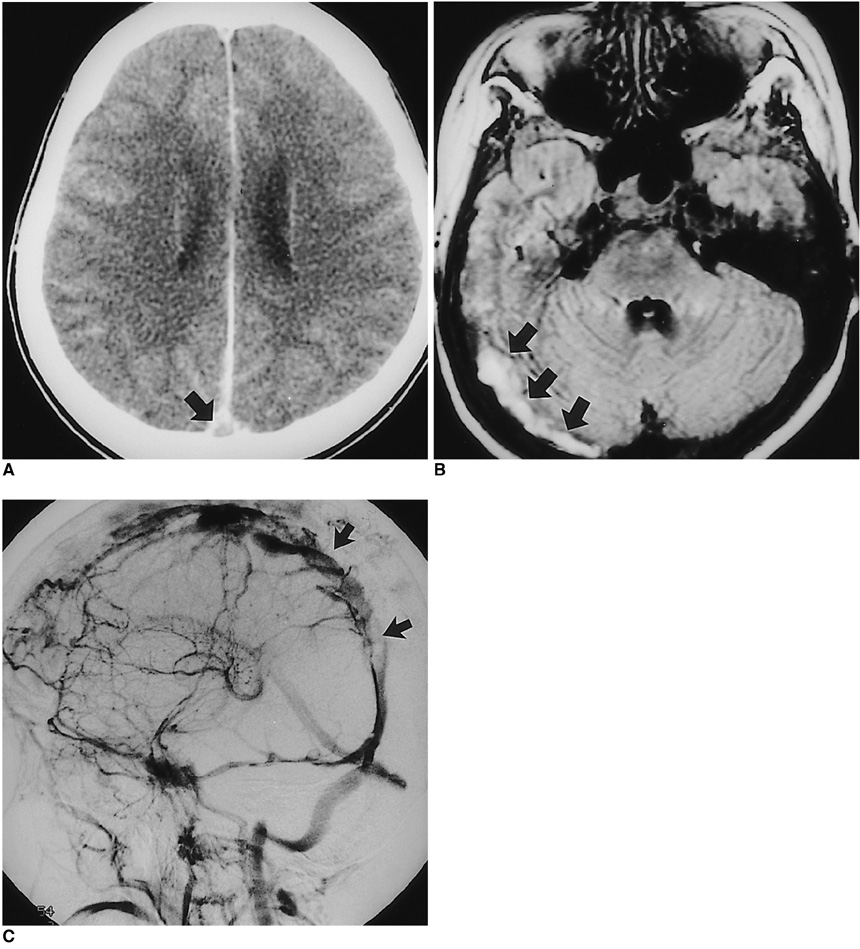
To describe the neuroradiologic findings of primary antiphospholipid antibody syndrome (PAPS). MATERIALS AND METHODS: During a recent two-year period, abnormally elevated antiphospholipid antibodies were detected in a total of 751 patients. In any cases in which risk factors for stroke were detected-hypertension, diabetes mellitus, hyperlipidemia, smoking, and the presence of SLE or other connective tissue diseases-PAPS was not diagnosed. Neuroradiologic studies were performed in 11 of 32 patients with PAPS. We retrospectively reviewed brain CT (n = 7), MR (n = 8), and cerebral angiography (n = 8) in 11 patients with special attention to the presence of brain parenchymal lesions and cerebral arterial or venous abnormalities. RESULTS: CT or MR findings of PAPS included nonspecific multiple hyper-inten-sity foci in deep white matter on T2-weighted images (5/11), a large infarct in the territory of the middle cerebral artery (4/11), diffuse cortical atrophy (2/11), focal hemorrhage (2/11), and dural sinus thrombosis (1/11). Angiographic findings were normal (5/8) or reflected either occlusion of a large cerebral artery (2/8) or dural sinus thrombosis (1/8). CONCLUSION: Neuroradiologic findings of PAPS are nonspecific but in young or middle-aged adults who show the above mentioned CT or MR findings, and in whom risk factors for stroke are not present, the condition should be suspected.
MeSH Terms
Figure
Reference
-
1. Harris EN, Gharavi AE, Hughes GRV. Antiphospholipid antibodies. Clin Rheum Dis. 1985. 11:591–609.2. Harris EN, Baguley E, Asherson RA, et al. Clinical and serological features of the "antiphospholipid syndrome". Br J Rheumatol. 1987. 26:S. 19.3. Hughson MD, Mccarty GA, Brumback RA. Spectrum of vascular pathology affecting patients with the antiphospholipid syndrome. Hum Pathol. 1995. 26:716–724.4. Asherson RA, Khamashta MA, Ordi-Ros J, et al. The "primary" antiphospholiupid syndrome: major clinical and serological features. Medicine. 1989. 68:366–374.5. Gharavi AE, Wilson WA. The syndrome of thrombosis, thrombocytopenia, and recurrent spontaneous abortions associated with antiphospholipid antibodies: Hughes syndrome. Lupus. 1996. 5:343–344.6. Provenzale JM, Heinz ER, Ortel TL, et al. Antiphospholipid antibodies in patients without SLE: neuroradiologic findings. Radiology. 1994. 192:531–537.7. Provenzale JM, Barboriak DP, Allen NB, Ortel TL. Patients with antiphospholipd antibodies: CT and MR findings of the brain. AJR. 1996. 167:1573–1578.8. Toubi E, Khamashta MA, Panarra A, Hugham GRV. Association of antiphospholipid antibodies with central nervous system disease in SLE. Am J Med. 1995. 99:397–401.9. Brey RL, Gharavi AE, Lockshin MD. Neurologic complications of antiphospholipid antibodies. Rheumatol Clin North Am. 1993. 4:833–850.10. Oeffinger KC, Roaten SP. Antihpospholipid syndrome. J Fam Prac. 1994. 38:611–619.11. Petri M. Pathogenesis and treatment of the antiphospholipid antibody syndrome. Med Clin North Am. 1997. 81:151–177.12. Aron AL, Gharavi AE, Shoenfeld Y. Mechanisms of action of antiphospholipid antibodies in the antiphospholipid antibodies in the antiphospholipd syndrome. Int Arch Allergy Immunol. 1995. 106:8–12.13. Lechner K, Pabinger-Fasching I. Lupus anticoagulants and thrombosis: a study of 25 cases and review of the literature. Haemostasis. 1985. 15:254–262.14. Levine SR, Brey RL. Neurological aspects of antihpospholipid antibody syndrome. Lupus. 1996. 5:347–353.15. Westerman EM, Miles JM. Neuropathologic findings in multi-infarct dementia associated with anticardiolipin antibody. Arthritis Rheum. 1992. 35:1038–1041.16. Coull BM, Bourdette DN, Goodnight SH, Briley DP, Hart R. Multiple cerebral infarctions and dementia as associated with anticardiolipin antibodies. Stroke. 1987. 18:1107–1112.17. Westerman EM, Miles KM, Backonja M, Sundstrom WR. Neuropahtologic findings in multi-infarct dementia associated with anticardiolipin antibody. Arthritis Rheum. 1992. 9:1038–1041.18. Levin SR, Kieran S, Puzio K, et al. Cerebral venous thrombosis with lupus anticoagulants: report of two cases. Stroke. 1987. 18:801–804.19. Carhuapoma JR, Mitsias P, Levine SR. Cerebral venous thrombosis and antiphospholipid antibodies. Stroke. 1997. 28:2363–2369.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A patient with chorea associated with hyperthyroidism and primary antiphospholipid antibody syndrome
- A Case of Primary Adrenal Insufficiency Presenting as the Initial Clinical Manifestation of Primary Antiphospholipid Antibody Syndrome
- A Case of Refractory Headache with Antiphospholipid Antibody Syndrome Improved by High-Intensity Warfarin Medication
- Flank ulcer in a patient with primary antiphospholipid syndrome
- Antiphospholipid Antibody Syndrome