Korean J Radiol.
2009 Aug;10(4):323-332. 10.3348/kjr.2009.10.4.323.
Head and Neck Vascular Lesions: Characterization of the Flow Pattern by the Use of Three-Phase CT
- Affiliations
-
- 1Department of Radiology, East-West Neomedical Center, Kyung Hee University, College of Medicine, Seoul 134-090, Korea.
- 2Department of Radiology, Seoul Veterans Hospital, Seoul 134-791, Korea.
- 3Department of Radiology and Research Institute of Radiology, University of Ulsan, College of Medicine, Asan Medical Center, Seoul 138-736, Korea. dcsuh@amc.seoul.kr
- KMID: 1777259
- DOI: http://doi.org/10.3348/kjr.2009.10.4.323
Abstract
OBJECTIVE
This study was designed to evaluate the usefulness of three-phase CT to characterize the hemodynamics of vascular lesions in the head and neck area.
MATERIALS AND METHODS
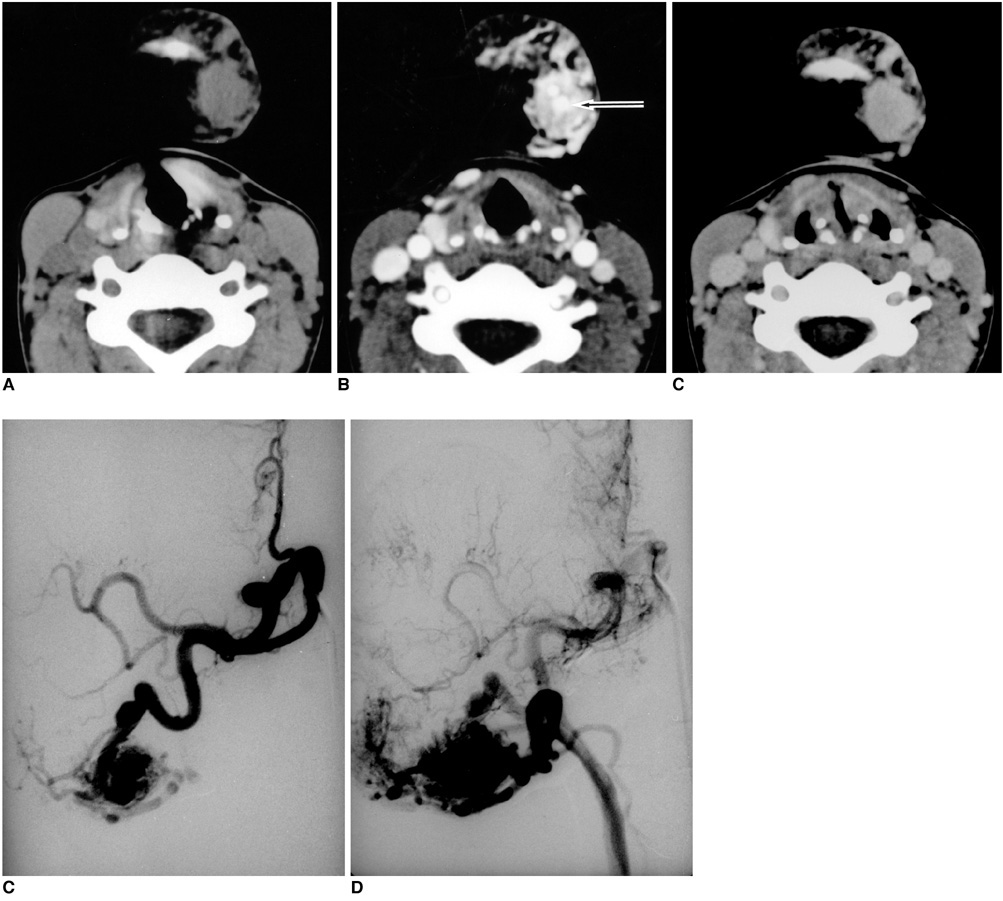
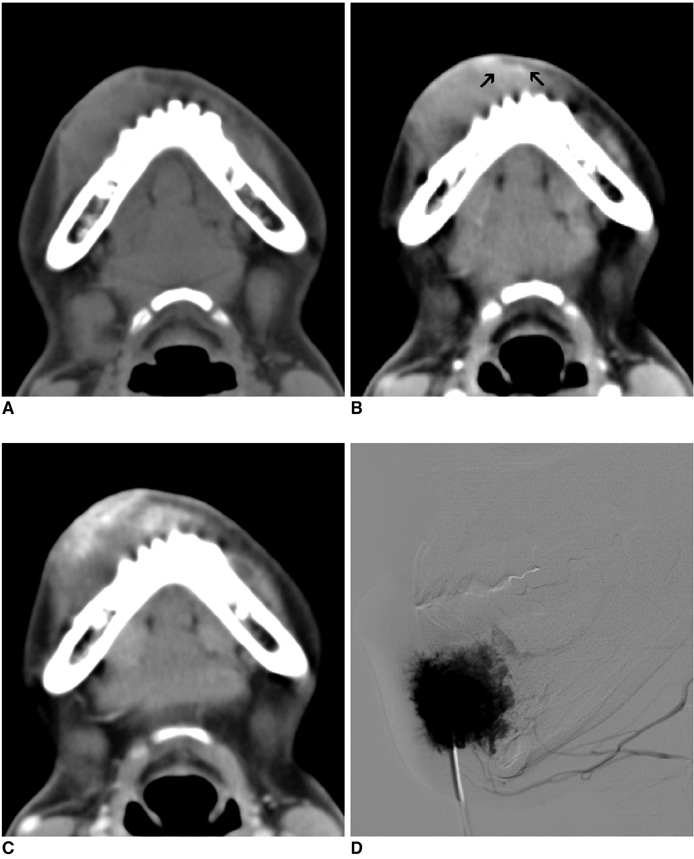
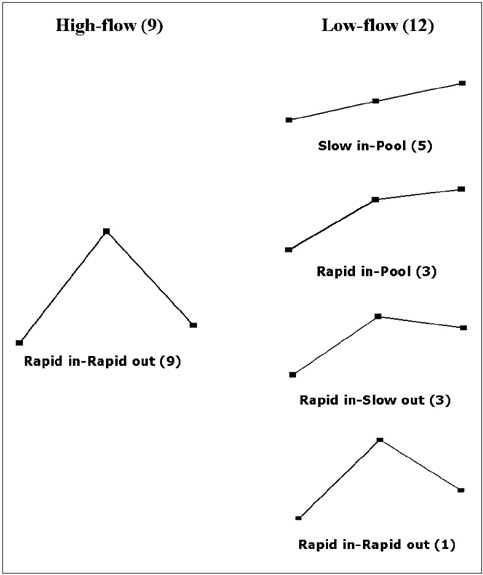
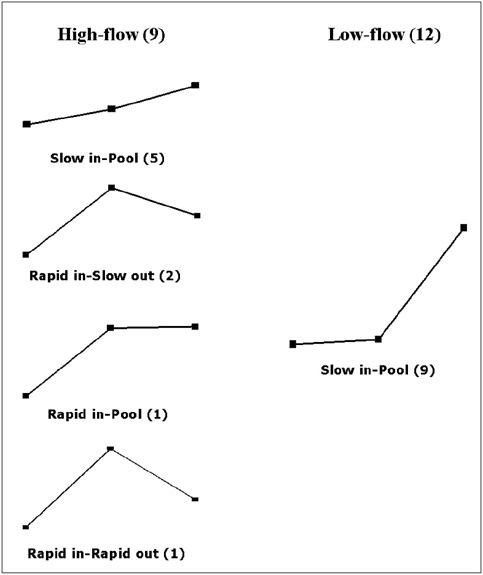
We analyzed vascular malformations of head and neck regions in 21 patients with the use of three-phase CT, including pre-contrast phase, vascular phase (scan delay: 20-35 seconds after intravenous contrast material injection) and equilibrium phase (scan delay: 3-5 minutes) imaging. The flow characteristic of each lesion was determined and categorized as either a high- or a low-flow lesion according to findings on selective arteriography and/or direct puncture venography. The CT number was acquired from two areas in a vascular lesion, sorted by the enhancement pattern: area 1, a highly enhanced area seen on the vascular phase; area 2, a delayedly enhanced area seen on the equilibrium phase. The CT numbers of each phase were compared between high- and low-flow lesions with use of the unpaired t-test. The flow patterns of high- and low-flow lesions were analyzed by assessment of time-density curves of three phase CT.
RESULTS
High-flow lesions were detected in nine patients and low-flow lesions were detected in 12 patients. On the vascular phase, the CT number of areas 1 and 2 of high-flow lesions was significantly higher than for low-flow lesions (p < 0.05). Contrary to early peaks seen in time-density curves of high-flow lesions, low-flow lesions showed a delayed peak.
CONCLUSION
Three-phase CT seems to be a valuable non-invasive method to differentiate a high-flow lesion from a low flow lesion of head and neck vascular lesions.
MeSH Terms
Figure
Cited by 1 articles
-
Visualization of Soft Tissue Venous Malformations of Head and Neck with 4D Flow Magnetic Resonance Imaging
Ji Ye Lee, Dae Chul Suh
Neurointervention. 2017;12(2):110-115. doi: 10.5469/neuroint.2017.12.2.110.
Reference
-
1. Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg. 1982. 69:412–422.2. Jackson IT, Carreno R, Potparic Z, Hussain K. Hemangiomas, vascular malformations, and lymphovenous malformations: classification and methods of treatment. Plast Reconstr Surg. 1993. 91:1216–1230.3. Burrows PE, Mulliken JB, Fellows KE, Strand RD. Childhood hemangiomas and vascular malformations: angiographic differentiation. AJR Am J Roentgenol. 1983. 141:483–488.4. Kaban LB, Mulliken JB. Vascular anomalies of the maxillofacial region. J Oral Maxillofac Surg. 1986. 44:203–213.5. Dubois JM, Sebag GH, De Prost Y, Teillac D, Chretien B, Brunelle FO. Soft-tissue venous malformations in children: percutaneous sclerotherapy with Ethibloc. Radiology. 1991. 180:195–198.6. Byun JH, Kim TK, Lee CW, Lee JK, Kim AY, Kim PN, et al. Arterioportal shunt: prevalence in small hemangiomas versus that in hepatocellular carcinomas 3 cm or smaller at two-phase helical CT. Radiology. 2004. 232:354–360.7. Sheafor DH, Frederick MG, Paulson EK, Keogan MT, DeLong DM, Nelson RC. Comparison of unenhanced, hepatic arterial-dominant, and portal venous-dominant phase helical CT for the detection of liver metastases in women with breast carcinoma. AJR Am J Roentgenol. 1999. 172:961–968.8. Kim KW, Kim TK, Han JK, Kim AY, Lee HJ, Choi BI. Hepatic hemangiomas with arterioportal shunt: findings at two-phase CT. Radiology. 2001. 219:707–711.9. Miller JD, Grace MG, Russell DB, Zacks DJ. Complications of cerebral angiography and pneumography. Radiology. 1977. 124:741–744.10. Cloft HJ, Joseph GJ, Dion JE. Risk of cerebral angiography in patients with subarachnoid hemorrhage, cerebral aneurysm, and arteriovenous malformation: a meta-analysis. Stroke. 1999. 30:317–320.11. Hill JH, Mafee MF, Chow JM, Applebaum EL. Dynamic computerized tomography in the assessment of hemangioma. Am J Otolaryngol. 1985. 6:23–28.12. Trop I, Dubois J, Guibaud L, Grignon A, Patriquin H, McCuaig C, et al. Soft-tissue venous malformations in pediatric and young adult patients: diagnosis with Doppler US. Radiology. 1999. 212:841–845.13. Fordham LA, Chung CJ, Donnelly LF. Imaging of congenital vascular and lymphatic anomalies of the head and neck. Neuroimaging Clin N Am. 2000. 10:117–136.14. Ziyeh S, Schumacher M, Strecker R, Rossler J, Hochmuth A, Klisch J. Head and neck vascular malformations: time-resolved MR projection angiography. Neuroradiology. 2003. 45:681–686.15. Dobson MJ, Hartley RW, Ashleigh R, Watson Y, Hawnaur JM. MR angiography and MR imaging of symptomatic vascular malformations. Clin Radiol. 1997. 52:595–602.16. van Rijswijk CS, van der Linden E, van der Woude HJ, van Baalen JM, Bloem JL. Value of dynamic contrast-enhanced MR imaging in diagnosing and classifying peripheral vascular malformations. AJR Am J Roentgenol. 2002. 178:1181–1187.17. Hopper KD, Neuman JD, King SH, Kunselman AR. Radioprotection to the eye during CT scanning. AJNR Am J Neuroradiol. 2001. 22:1194–1198.18. Namasivayam S, Kalra MK, Pottala KM, Waldrop SM, Hudgins PA. Optimization of Z-axis automatic exposure control for multidetector row CT evaluation of neck and comparison with fixed tube current technique for image quality and radiation dose. AJNR Am J Neuroradiol. 2006. 27:2221–2225.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vascular anomalies of the head and neck: current overview
- Imaging diagnosis of venous malformation in head and neck
- Velocity Window for Detection of Flow with MR Phase Imaging
- Establishment and Characterization of a Novel Cell Line (PNUH-12) Derived from a Human Squamous Cell Carcinoma of the Hypopharynx
- Clinical analysis of cystic lesions of the head and neck