Yonsei Med J.
2006 Dec;47(6):799-804. 10.3349/ymj.2006.47.6.799.
The CobraPLA(TM) During Anesthesia with Controlled Ventilation: A Clinical Trial of Efficacy
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine and Anesthesia and Pain Research Institute, Yonsei University College of Medicine, Seoul, Korea. jonglee@ yumc.yonsei.ac.kr
- KMID: 1777168
- DOI: http://doi.org/10.3349/ymj.2006.47.6.799
Abstract
- The CobraPLA(TM) (CPLA) is a relatively new supraglottic airway device that has not been sufficiently investigated. Here, we performed a prospective observational study to evaluate the efficacy of the CPLA during controlled ventilation. In 50 anesthetized and paralyzed patients undergoing elective surgery a CPLA was inserted and inflated to an intracuff pressure of 60 cm H2O. The success rate of insertion upon the first attempt was 82% (41/50), with a mean insertion time of 16.3 +/- 4.5 seconds. The adequacy of ventilation was assessed by observing the end tidal CO2 waveform, movement of the chest wall, peak airway pressure (13.5 cm H2O), and leak fraction (4%). We documented the airway sealing pressure (22.5 cm H2O) and noted that the the site of gas leaks at that pressure were either at the neck (52%), the abdomen (46%), or both (2%). In 44 (88%) patients, the vocal cords were visible in the fiberoptic view through the CPLA. There was no gastric insufflation during the anesthesia. Respiratory and hemodynamic parameters remained stable during CPLA insertion. Postoperative blood staining of CPLA was minimal, occurring in 22% (11/50) of patients. Mild and moderate throat soreness was reported in 44% (22/50) and 4% (2/50) of patients, respectively. Lastly, mild dysphonia was observed in 6% (3/50) of patients and mild dysphagia in 10% (5/50) of patients. Our results indicated that the CPLA is both easy to place and allows adequate ventilation during controlled ventilation.
MeSH Terms
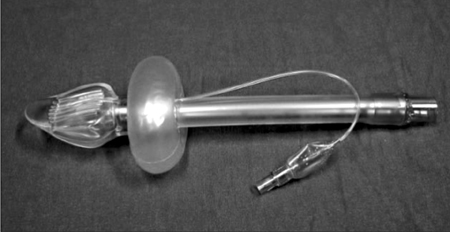
Figure
Reference
-
1. Brain AI. The laryngeal mask - a new concept in airway management. Br J Anaesth. 1983. 55:801–805.2. Brain AI. Three cases of difficult intubation overcome by the laryngeal mask airway. Anaesthesia. 1985. 40:353–355.3. Frass M, Frenzer R, Rauscha F, Weber H, Pacher R, Leithner C. Evaluation of esophageal tracheal combitube in cardiopulmonary resuscitation. Crit Care Med. 1987. 15:609–611.4. Devitt JH, Wenstone R, Noel AG, O'Donnell MP. The laryngeal mask airway and positive-pressure ventilation. Anesthesiology. 1994. 80:550–555.5. Cook TM, McKinstry C, Hardy R, Twigg S. Randomized crossover comparison of the ProSeal™ laryngeal mask airway with the Laryngeal Tube® during anaesthesia with controlled ventilation. Br J Anaesth. 2003. 91:678–683.6. Figueredo E, Martinez M, Pintanel T. A comparison of the ProSeal™ laryngeal mask and the laryngeal tube® in spontaneously breathing anesthetized patients. Anesth Analg. 2003. 96:600–605.7. Chiu CL, Murugasu J, Chan L. The use of modified VBM laryngeal tube compared to Laryngeal Mask Airway during spontaneous ventilation. Anaesth Intensive Care. 2003. 31:187–192.8. Akca O, Wadhwa A, Sengupta P, Durrani J, Hanni K, Wenke M, et al. The new perilaryngeal airway (CobraPLA™) is as efficient as the laryngeal mask airway (LMA™) but provides better airway sealing pressures. Anesth Analg. 2004. 99:272–278.9. Agro F, Barzoi G, Carassiti M, Galli B. Getting the tube in the oesophagus and oxygen in the trachea: preliminary results with the new supraglottic device (Cobra™) in 28 anaesthetised patients. Anaesthesia. 2003. 58:920–921.10. Lee KY, Chang CH, Nam SB, Shim YH, Lee CH, Lee JS. Efficacy of the laryngeal tube in general anesthesia. Korean J Anesthesiol. 2003. 45:687–692.11. Brimacombe J, Berry A. A proposed fiber-optic scoring system to standardize the assessment of laryngeal mask airway position. Anesth Analg. 1993. 76:457.12. Agro F, Barzoi G, Galli B. The CobraPLA™ in 110 anaesthetized and paralysed patients: what size to choose? Br J Anaesth. 2004. 92:777–778.13. Gaitini LA, Somri MJ, Kersh K, Yanovski B, Vaida S. A comparision of the Laryngeal mask airway unique™, pharyngeal airway X press™ and perilaryngeal airway cobra™ in paralyzed anesthetized adult patients. Anesthesiology. 2003. 99:A1495.14. Dorges V, Ocker H, Wenzel V, Schmucker P. The larygeal tube: a new simple airway device. Anesth Analg. 2000. 90:1220–1222.15. Ocker H, Wenzel V, Schmucker P, Steinfath M, Dorges V. A comparison of the laryngeal tube with the laryngeal mask airway during routine surgical procedures. Anesth Analg. 2002. 95:1094–1097.16. Stanley TH, Kawamura R, Graves C. Effects of nitrous oxide on volume and pressure of endotracheal tube cuffs. Anesthesiology. 1974. 41:256–262.17. Karasawa F, Ohshima T, Takamatsu I, Ehata T, Fukuda I, Uchihashi Y, et al. The effect on intracuff pressure of various nitrous oxide concentrations used for inflating an endotracheal tube cuff. Anesth Analg. 2000. 91:708–713.18. Brimacombe J, Keller C, Puhringer F. Pharyngeal mucosal pressure and perfusion: a fiberoptic evaluation of the posterior pharynx in anesthetized adult patients with a modified cuffed oropharyngeal airway. Anesthesiology. 1999. 91:1661–1665.19. Tu HN, Saidi N, Lieutaud T, Bensaid S, Menival V, Duvaldestin P. Nitrous oxide increases endotracheal cuff pressure and the incidence of tracheal lesions in anesthetized patients. Anesth Analg. 1999. 89:187–190.20. Gaitini LA, Vaida SJ, Somri M, Kaplan V, Yanovski B, Markovits R, et al. An evaluation of the Laryngeal Tube during general anesthesia using mechanical ventilation. Anesth Analg. 2003. 96:1750–1755.21. Dich-Nielsen JO, Nagel P. Flexible fibreoptic bronchoscopy via the laryngeal mask. Acta Anaesthesiol Scand. 1993. 37:17–19.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of the CobraPLA and the LMA Classic airway devices during volume-controlled ventilation in children
- Effects of Manually Controlled Ventilation on Gas Exchange during General Anesthesia
- A clinical evaluation of i-gel(TM) during general anesthesia in children
- Clinical performance of Ambu AuraGainTM versus i-gelTM in anesthetized children: a prospective, randomized controlled trial
- Arterial Blood Gas Analysis Following Ventilatory Patterns