Korean J Gastroenterol.
2009 Dec;54(6):409-412. 10.4166/kjg.2009.54.6.409.
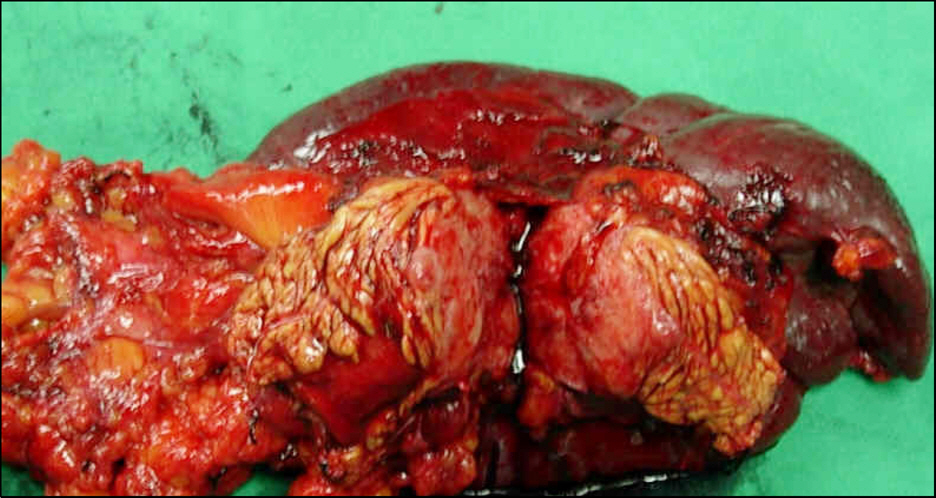
Paraganglioma of the Pancreas Metastasized to the Adrenal Gland: A Case Report
- Affiliations
-
- 1Department of Surgery, Kepco Medical Foundation, Hanil General Hospital, Seoul, Korea. kpaik@ymail.com
- KMID: 1775943
- DOI: http://doi.org/10.4166/kjg.2009.54.6.409
Abstract
- Paraganglioma is a rare neuroendocrine tumor arising from the neural crest, which includes tissues such as the adrenal medulla, carotid and aortic body, organs of Zuckerkandl, and other unnamed paraganglia. The head, neck, and retroperitoneum are the most common sites for paraganglioma. However, paraganglioma of the pancreas is extremely rare. We report our experience of this rare disease. A 70-year old female patient admitted for a pancreas tail mass detected by computed tomography (CT) scan checked for vague left flank pain. CT with contrast enhancement showed a 4.2-cm heterogeneously enhanced lesion in the tail of the pancreas. A well defined ovoid shape mass in left adrenal gland was suggested adenoma. Distal pancreatectomy with left adrenalectomy was performed. Any lymph node enlargement was not found. Pancreas mass did not invade adjacent organ. Microscopic examination with pancreas and adrenal gland revealed that the cells were arranged in a characteristic Zellballen pattern. Immunohistochemical staining revealed positivity for neuron-specific enolase, chromogranin A, synaptophysin, and S-100 protein. On the basis of these findings, we diagnosed the tumor as a paraganglioma of the pancreas and adrenal gland. We report the first case of pancreas paraganglioma in Korea.
Keyword
MeSH Terms
-
Adenoma/diagnosis/surgery
Adrenal Gland Neoplasms/*diagnosis/secondary/surgery
Aged
Chromogranin A/metabolism
Female
Humans
Pancreatic Neoplasms/*diagnosis/pathology/surgery
Paraganglioma/*diagnosis/secondary/surgery
Phosphopyruvate Hydratase/metabolism
S100 Proteins/metabolism
Synaptophysin/metabolism
Tomography, X-Ray Computed
Figure
Reference
-
1. DeLellis RA, Lloyd RV, Heitz PU. Tumours of endocrine organs. Lyon: IARC Press;2004.2. Sclafani LM, Woodruff JM, Brennan MF. Extraadrenal retroperitoneal paragangliomas: natural history and response to treatment. Surgery. 1990; 108:1124–1130.3. Tsukada A, Ishizaki Y, Nobukawa B, Kawasaki S. Paraganglioma of the pancreas: a case report and review of the literature. Pancreas. 2008; 36:214–216.4. Lack EE. Tumours of adrenal and extraadrenal paraganglia. Solae G, editor. ed.Histological typing of endocrine tumors. 2nd ed.Berlin: Springer;2000. p. 38–48.5. Fries JG, Chamberlin JA. Extraadrenal pheochromocytoma: literature review and report of a cervical pheochromocytoma. Surgery. 1968; 63:268–279.6. Lloyd RV, Tischer AS, Kimura N, et al. Adrenal tumors: introduction. DeLellis RA, editor. ed.World health organization classification of tumours: pathology and genetics of tumours of endocrine organs. Lyon: IARC Press;2004. p. 136–138.7. Whalen RK, Althausen AF, Daniels GH. Extraadrenal pheochromocytoma. J Urol. 1992; 147:1–10.
Article8. Beard CM, Sheps SG, Kurland LT, et al. Occurrence of pheochromocytoma in Rochester, Minnesota, 1950 through 1979. Mayo Clin Proc. 1983; 58:802–804.9. Young WF. Paragangliomas: clinical overview. Ann NY Acad Sci. 2006; 1073:21–29.
Article10. Erickson D, Kudva YC, Ebersold MJ, et al. Benign paragangliomas: clinical presentation and treatment outcomes in 236 patients. J Clin Endocrinol Metab. 2001; 86:5210–5216.
Article11. Bartley O, Ekdahl PH, Hulten L. Paraganglioma simulating pancreatic cyst. Report of two cases. Acta Chir Scand. 1966; 132:289–297.12. Cope C, Greenberg SH, Vidal JJ, et al. Nonfunctioning nonchromaffin paraganglioma of the pancreas. Arch Surg. 1974; 109:440–442.
Article13. Zamir O, Amir G, Lemau O, et al. Nonfunctional paraganglioma of the pancreas. Am J Gastroenterol. 1984; 79:761–763.14. Fujino Y, Nagata Y, Ogino K, et al. Nonfunctional paraganglioma of the pancreas: report of a case. Surg Today. 1998; 28:209–212.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Extra-adrenal Paraganglioma of the Retroperitoneum
- A Case of Extra-adrenal Paraganglioma of the Scrotum
- Ultrasound, CT, and MR imaging Findings of Paraganglioma Originating at the Urinary Bladder: A Case Report
- Malignant Gastric Paraganglioma with Liver Metastasis: Imaging Findings and Literature Review
- Composite Pheochromocytoma or Paraganglioma of Adrenal Gland: A Case Report with Immunohistochemical Studies and Electron Microscopic Examination