Korean J Gastroenterol.
2009 Dec;54(6):395-398. 10.4166/kjg.2009.54.6.395.
A Case of Spontaneous Pneumoperitoneum Associated with Idiopathic Intestinal Pseudoobstruction
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. HJPARK21@yuhs.ac
- KMID: 1775940
- DOI: http://doi.org/10.4166/kjg.2009.54.6.395
Abstract
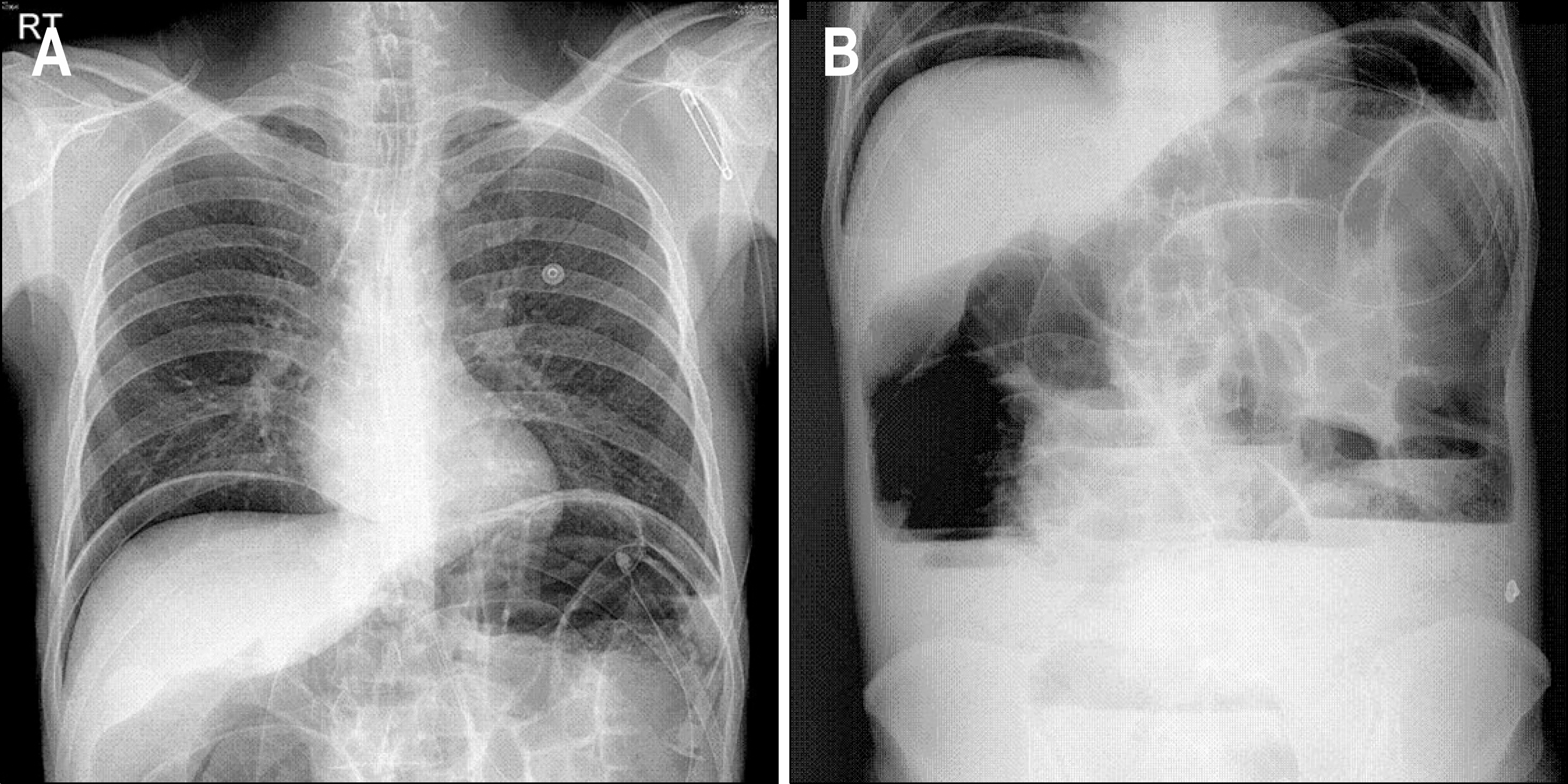
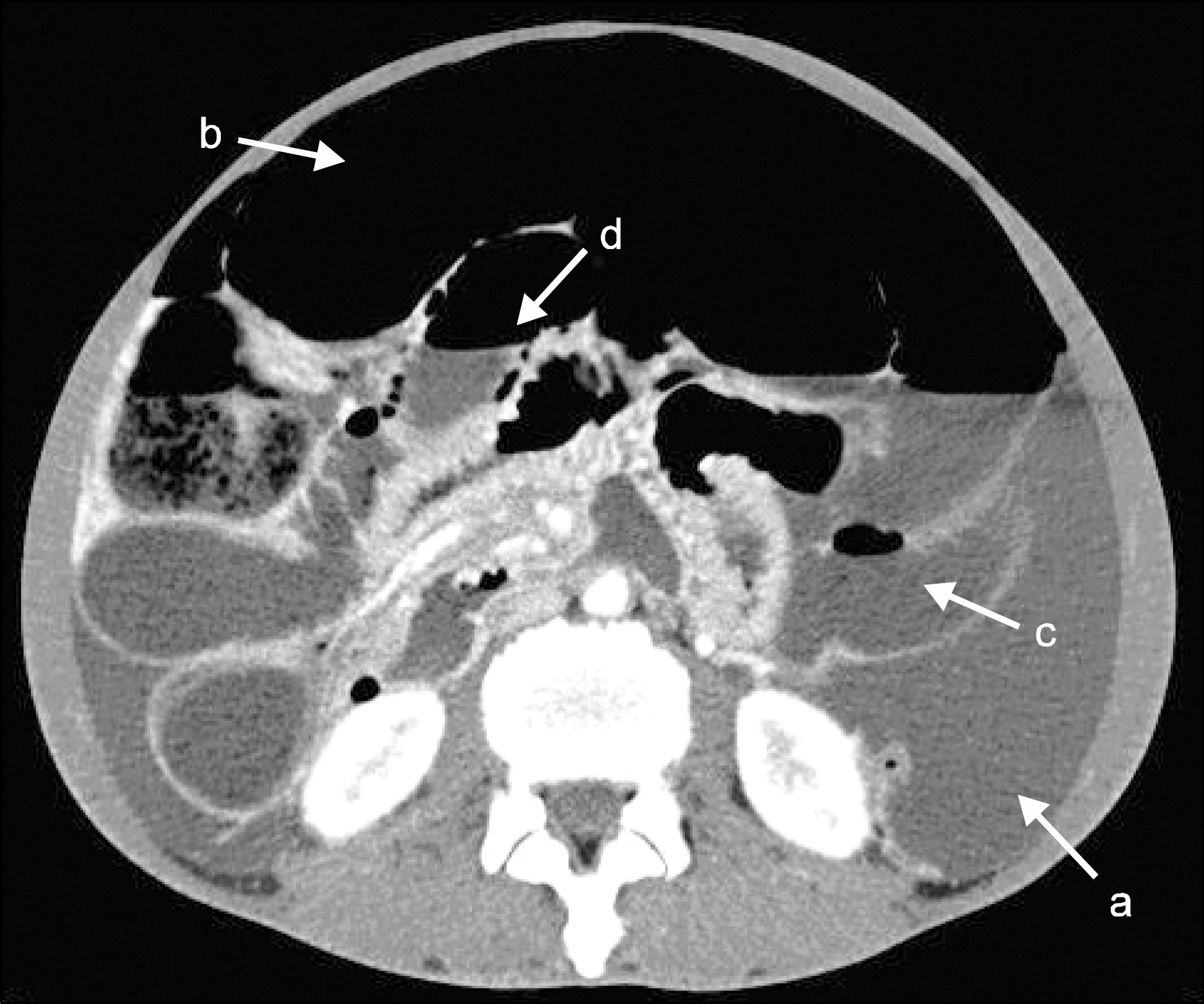
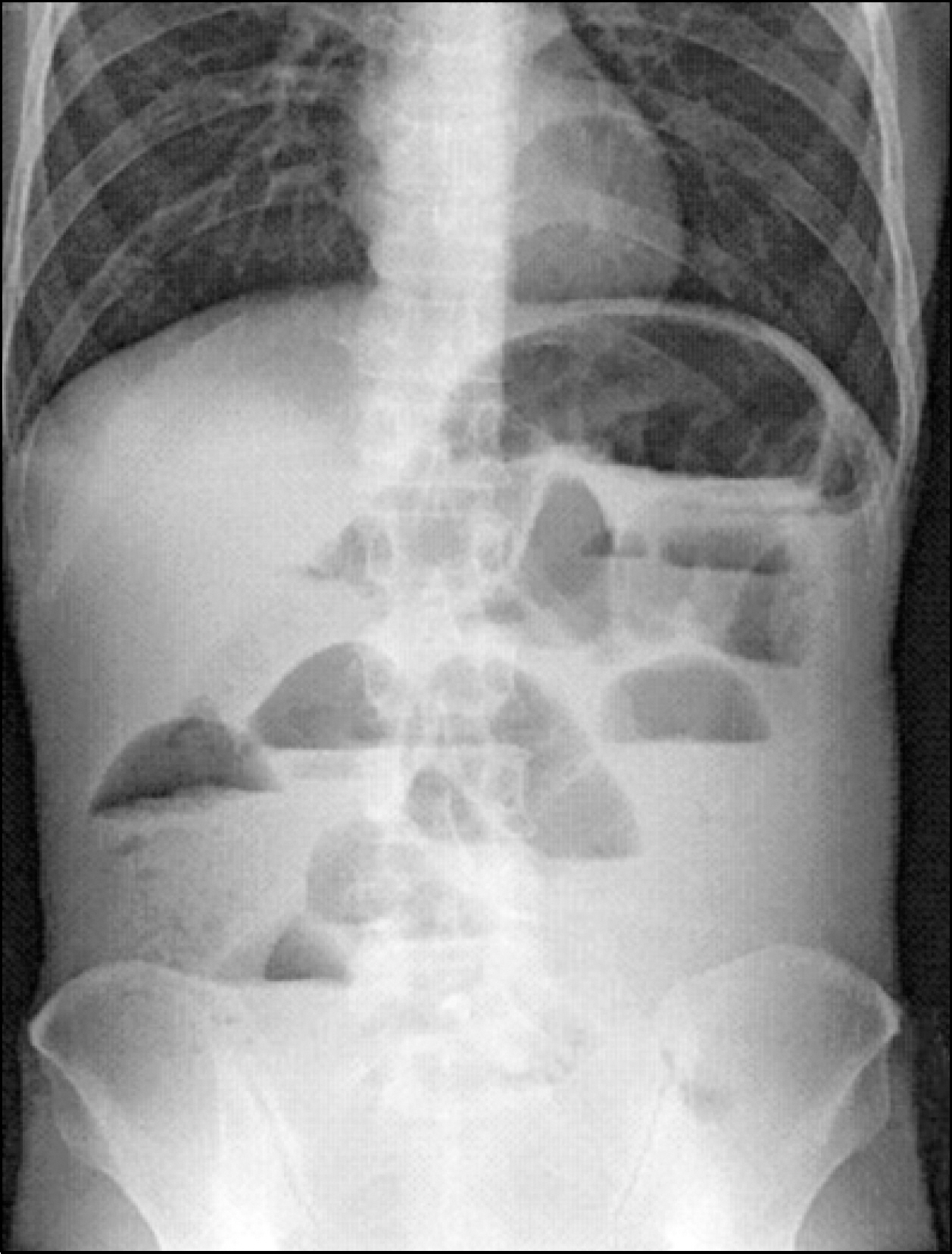
- Pneumoperitoneum, free intra-abdominal air, usually results from the perforation of a hollow viscous. In approximately 10% of cases, however, pneumoperitoneum is not caused by gastrointestinal perforation. These cases of "spontaneous pneumoperitoneum" generally follow more benign course and may not require surgical intervention. Examples include cardiopulmonary resuscitation (CPR), malrotation, mechanical ventilator support, gynecologic manipulation, blunt abdominal trauma, and chronic intestinal pseudoobstruction in infancy (Sieber syndrome). But, it is extremely rare of spontaneous pneumoperitoneum secondary to idiopathic intestinal pseudoobstuction in adult. We herein report a patient with chronic idiopathic intestinal pseudoobstuction who developed a pneumoperitoneum.
MeSH Terms
Figure
Reference
-
1. Mason JM, Mason EM, Kesmodel KF. Spontaneous pneumoperitoneum without peritonitis and without demonstrable cause. In: Tani T, Shirai Y, Sasagawa M, et al. Conservative management of idiopathic pneumoperitoneum masquerading as peritonitis: report a case. Jpn J Surg. 1995; 25:265–267.2. Mularski RA, Sippel JM, Osborne ML. Pneumoperitoneum: a review of nonsurgical causes. Crit Care Med. 2000; 28:26392644.
Article3. Williams NMA, Watkin DFL. Spontaneous pneumoperitoneum and other nonsurgical causes of intraperitoneal free gas. Postgrad Med J. 1997; 73:531–537.
Article4. Winer-Muram HT, Rumbak MJ, Bain RS Jr. Tension pneumoperitoneum as a complication of barotrauma. Crit Care Med. 1993; 21:941–943.
Article5. Chitchley LA, Rowbottom S. Fatal tension pneumoperitoneum with pneumothorax. Anaesth Intensive Care. 1994; 22:298–299.
Article6. Johnson EK, Choi YU, Jarrard SW, Rivera D. Pneumoperitoneum after rough sexual intercourse. Am Surg. 2002; 68:430–433.7. Gensburg RS, Wojcik WG, Mehta SD. Vaginally-induced pneumoperitoneum during pregnancy. Am J Radiology. 1988; 150:595–596.8. Knechtle SJ, Davidoff AM, Rice RP. Pneumatosis intestinalis. Surgical management and clinical outcome. Ann Surg. 1990; 212:161–165.9. Shiba H, Aoki H, Misawa T, Kobayashi S, Saito R, Yanaga K. Pneumoperitoneum caused by ruptured gas-containing liver abscess. J Hepatobiliary Pancreat Surg. 2007; 14:210–211.
Article10. Pidala MJ, Slezak FA, Porter JA. Pneumoperitoneum following percutanous endoscopic gastrostomy: does the timing of pan-endoscopy matter? Surg Endosc. 1992; 6:128–129.11. Prasannan S, Kumar S, Gul YA. Spontaneous pneumoperitoneum associated with colonic pseudoobstruction. Acta Chir Belg. 2004; 104:739–741.
Article12. Derveaux K, Penninckx F. Recurrent “spontaneous” pneumoperitoneum: a diagnostic and therapeutic dilemma. Acta Chir Belg. 2003; 103:490–492.
Article13. Karaman A, Demirbilek S, Akin M, Gurunluoglu K, Irsi C. Does pneumoperitoneum always require laparotomy? Report of six cases and review of the literature. Pediatr Surg Int. 2005; 21:819–824.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Idiopathic Pneumoperitoneum in a Premature Infant
- A Case of Chronic Idiopathic Intestinal Pseudoobstruction
- A Case of Intestinal Pseudoobstruction with Positive Serum Anti - Hu Antibody in Small Cell Lung Carcinoma
- Intestinal Pseudoobstruction Caused by Chronic Lyme Neuroborreliosis. A Case Report
- Spontaneous Perforation of Small Bowel Lymphoma Causing Massive Pneumoperitoneum: A case Report