Korean J Gastroenterol.
2012 Jan;59(1):1-7. 10.4166/kjg.2012.59.1.1.
Obesity and Functional Gastrointestinal Disorders
- Affiliations
-
- 1Department of Internal Medicine, Ajou University School of Medicine, Suwon, Korea. kjleemd@hotmail.com
- KMID: 1775826
- DOI: http://doi.org/10.4166/kjg.2012.59.1.1
Abstract
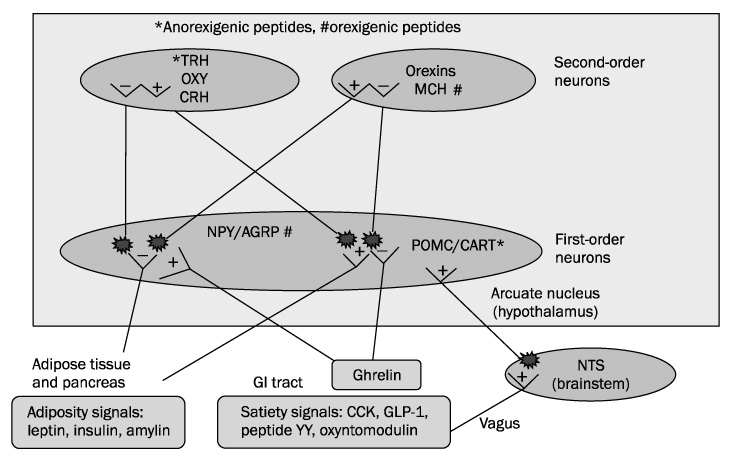
- Obesity is prevalent in Korea. An increase in food intake and a decrease in energy expenditure are responsible for obesity. Gut hormones play a role in controlling food intake. Obesity is suggested to be linked to common gastrointestinal functional disorders. Obesity is associated with an increased risk of gastroesophageal reflux disease, Barrett esophagus and esophageal adenocarcinoma. Epidemiologic studies indicate that obesity is associated with chronic gastrointestinal symptoms. This association suggests the possibility that obesity and functional gastrointestinal disorders may be pathophysiologically linked. However, data on the relationship between obesity and functional gastrointestinal disorders are inconsistent. In this paper, we review the role of gastrointestinal hormones in food intake and the relationship between obesity and functional gastrointestinal disorders.
MeSH Terms
Figure
Cited by 2 articles
-
Gastrointestinal Gas and Abdominal Fat Quantity Measured by Three-Dimensional Abdominal Computed Tomography in Patients with Functional Bloating
Hong Sub Lee, Jai Keun Kim, Joo Sung Sun, Kwang Jae Lee
Korean J Gastroenterol. 2018;71(6):324-331. doi: 10.4166/kjg.2018.71.6.324.비만과 상부 위장관 질환
Younghee Choe
Korean J Gastroenterol. 2024;83(3):81-86. doi: 10.4166/kjg.2024.015.
Reference
-
1. Valassi E, Scacchi M, Cavagnini F. Neuroendocrine control of food intake. Nutr Metab Cardiovasc Dis. 2008. 18:158–168.2. Neary MT, Batterham RL. Gut hormones: implications for the treatment of obesity. Pharmacol Ther. 2009. 124:44–56.3. Suzuki K, Simpson KA, Minnion JS, Shillito JC, Bloom SR. The role of gut hormones and the hypothalamus in appetite regulation. Endocr J. 2010. 57:359–372.4. Wren AM, Seal LJ, Cohen MA, et al. Ghrelin enhances appetite and increases food intake in humans. J Clin Endocrinol Metab. 2001. 86:5992.5. Levin F, Edholm T, Schmidt PT, et al. Ghrelin stimulates gastric emptying and hunger in normal-weight humans. J Clin Endocrinol Metab. 2006. 91:3296–3302.6. Monti V, Carlson JJ, Hunt SC, Adams TD. Relationship of ghrelin and leptin hormones with body mass index and waist circumference in a random sample of adults. J Am Diet Assoc. 2006. 106:822–828.7. Lawrence CB, Snape AC, Baudoin FM, Luckman SM. Acute central ghrelin and GH secretagogues induce feeding and activate brain appetite centers. Endocrinology. 2002. 143:155–162.8. Jéquier E. Leptin signaling, adiposity, and energy balance. Ann N Y Acad Sci. 2002. 967:379–388.9. Munzberg H. Leptin-signaling pathways and leptin resistance. Forum Nutr. 2010. 63:123–132.10. Air EL, Benoit SC, Clegg DJ, Seeley RJ, Woods SC. Insulin and leptin combine additively to reduce food intake and body weight in rats. Endocrinology. 2002. 143:2449–2452.11. Lutz TA. Amylinergic control of food intake. Physiol Behav. 2006. 89:465–471.12. Hollander PA, Levy P, Fineman MS, et al. Pramlintide as an adjunct to insulin therapy improves long-term glycemic and weight control in patients with type 2 diabetes: a 1-year randomized controlled trial. Diabetes Care. 2003. 26:784–790.13. Ueno N, Inui A, Iwamoto M, et al. Decreased food intake and body weight in pancreatic polypeptide-overexpressing mice. Gastroenterology. 1999. 117:1427–1432.14. Lieverse RJ, Masclee AA, Jansen JB, Rovati LC, Lamers CB. Satiety effects of the type A CCK receptor antagonist loxiglumide in lean and obese women. Biol Psychiatry. 1995. 37:331–335.15. Lieverse RJ, Jansen JB, Masclee AA, Lamers CB. Satiety effects of a physiological dose of cholecystokinin in humans. Gut. 1995. 36:176–179.16. Jordan J, Greenway FL, Leiter LA, et al. Stimulation of cholecystokinin-A receptors with GI181771X does not cause weight loss in overweight or obese patients. Clin Pharmacol Ther. 2008. 83:281–287.17. Abbott CR, Monteiro M, Small CJ, et al. The inhibitory effects of peripheral administration of peptide YY(3-36) and glucagon-like peptide-1 on food intake are attenuated by ablation of the vagal-brainstem-hypothalamic pathway. Brain Res. 2005. 1044:127–131.18. Kim D, MacConell L, Zhuang D, et al. Effects of once-weekly dosing of a long-acting release formulation of exenatide on glucose control and body weight in subjects with type 2 diabetes. Diabetes Care. 2007. 30:1487–1493.19. Cohen MA, Ellis SM, Le Roux CW, et al. Oxyntomodulin suppresses appetite and reduces food intake in humans. J Clin Endocrinol Metab. 2003. 88:4696–4701.20. Wynne K, Park AJ, Small CJ, et al. Subcutaneous oxyntomodulin reduces body weight in overweight and obese subjects: a double-blind, randomized, controlled trial. Diabetes. 2005. 54:2390–2395.21. Batterham RL, Cowley MA, Small CJ, et al. Gut hormone PYY (3-36) physiologically inhibits food intake. Nature. 2002. 418:650–654.22. Abbott CR, Small CJ, Kennedy AR, et al. Blockade of the neuropeptide Y Y2 receptor with the specific antagonist BIIE0246 attenuates the effect of endogenous and exogenous peptide YY(3-36) on food intake. Brain Res. 2005. 1043:139–144.23. Yang SY, Lee OY, Bak YT, et al. Prevalence of gastroesophageal reflux disease symptoms and uninvestigated dyspepsia in Korea: a population-based study. Dig Dis Sci. 2008. 53:188–193.24. Lee SY, Lee KJ, Kim SJ, Cho SW. Prevalence and risk factors for overlaps between gastroesophageal reflux disease, dyspepsia, and irritable bowel syndrome: a population-based study. Digestion. 2009. 79:196–201.25. El-Serag HB, Graham DY, Satia JA, Rabeneck L. Obesity is an independent risk factor for GERD symptoms and erosive esophagitis. Am J Gastroenterol. 2005. 100:1243–1250.26. Jacobson BC, Somers SC, Fuchs CS, Kelly CP, Camargo CA Jr. Body-mass index and symptoms of gastroesophageal reflux in women. N Engl J Med. 2006. 354:2340–2348.27. Iovino P, Angrisani L, Galloro G, et al. Proximal stomach function in obesity with normal or abnormal oesophageal acid exposure. Neurogastroenterol Motil. 2006. 18:425–432.28. Nocon M, Labenz J, Willich SN. Lifestyle factors and symptoms of gastro-oesophageal reflux-a population-based study. Aliment Pharmacol Ther. 2006. 23:169–174.29. El-Serag HB, Ergun GA, Pandolfino J, Fitzgerald S, Tran T, Kramer JR. Obesity increases oesophageal acid exposure. Gut. 2007. 56:749–755.30. El-Serag HB, Kvapil P, Hacken-Bitar J, Kramer JR. Abdominal obesity and the risk of Barrett's esophagus. Am J Gastroenterol. 2005. 100:2151–2156.31. Freeman HJ. Risk of gastrointestinal malignancies and mechanisms of cancer development with obesity and its treatment. Best Pract Res Clin Gastroenterol. 2004. 18:1167–1175.32. Veugelers PJ, Porter GA, Guernsey DL, Casson AG. Obesity and lifestyle risk factors for gastroesophageal reflux disease, Barrett esophagus and esophageal adenocarcinoma. Dis Esophagus. 2006. 19:321–328.33. Edelstein ZR, Farrow DC, Bronner MP, Rosen SN, Vaughan TL. Central adiposity and risk of Barrett's esophagus. Gastroenterology. 2007. 133:403–411.34. Iovino P, Angrisani L, Tremolaterra F, et al. Abnormal esophageal acid exposure is common in morbidly obese patients and improves after a successful Lap-band system implantation. Surg Endosc. 2002. 16:1631–1635.35. Wu JC, Mui LM, Cheung CM, Chan Y, Sung JJ. Obesity is associated with increased transient lower esophageal sphincter relaxation. Gastroenterology. 2007. 132:883–889.36. Pandolfino JE, El-Serag HB, Zhang Q, Shah N, Ghosh SK, Kahrilas PJ. Obesity: a challenge to esophagogastric junction integrity. Gastroenterology. 2006. 130:639–649.37. Koppman JS, Poggi L, Szomstein S, Ukleja A, Botoman A, Rosenthal R. Esophageal motility disorders in the morbidly obese population. Surg Endosc. 2007. 21:761–764.38. Suter M, Dorta G, Giusti V, Calmes JM. Gastro-esophageal reflux and esophageal motility disorders in morbidly obese patients. Obes Surg. 2004. 14:959–966.39. Quiroga E, Cuenca-Abente F, Flum D, Dellinger EP, Oelschlager BK. Impaired esophageal function in morbidly obese patients with gastroesophageal reflux disease: evaluation with multichannel intraluminal impedance. Surg Endosc. 2006. 20:739–743.40. Frederiksen SG, Johansson J, Johnsson F, Hedenbro J. Neither low-calorie diet nor vertical banded gastroplasty influence gastro-oesophageal reflux in morbidly obese patients. Eur J Surg. 2000. 166:296–300.41. Kjellin A, Ramel S, Rössner S, Thor K. Gastroesophageal reflux in obese patients is not reduced by weight reduction. Scand J Gastroenterol. 1996. 31:1047–1051.42. Fraser-Moodie CA, Norton B, Gornall C, Magnago S, Weale AR, Holmes GK. Weight loss has an independent beneficial effect on symptoms of gastro-oesophageal reflux in patients who are overweight. Scand J Gastroenterol. 1999. 34:337–340.43. Frezza EE, Ikramuddin S, Gourash W, et al. Symptomatic improvement in gastroesophageal reflux disease (GERD) following laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2002. 16:1027–1031.44. Lara MD, Kothari SN, Sugerman HJ. Surgical management of obesity: a review of the evidence relating to the health benefits and risks. Treat Endocrinol. 2005. 4:55–64.45. van Oijen MG, Josemanders DF, Laheij RJ, van Rossum LG, Tan AC, Jansen JB. Gastrointestinal disorders and symptoms: does body mass index matter? Neth J Med. 2006. 64:45–49.46. Delgado-Aros S, Locke GR 3rd, Camilleri M, et al. Obesity is associated with increased risk of gastrointestinal symptoms: a population-based study. Am J Gastroenterol. 2004. 99:1801–1806.47. Talley NJ, Quan C, Jones MP, Horowitz M. Association of upper and lower gastrointestinal tract symptoms with body mass index in an Australian cohort. Neurogastroenterol Motil. 2004. 16:413–419.48. Talley NJ, Howell S, Poulton R. Obesity and chronic gastrointestinal tract symptoms in young adults: a birth cohort study. Am J Gastroenterol. 2004. 99:1807–1814.49. Aro P, Ronkainen J, Talley NJ, Storskrubb T, Bolling-Sternevald E, Agréus L. Body mass index and chronic unexplained gastrointestinal symptoms: an adult endoscopic population based study. Gut. 2005. 54:1377–1383.50. Cardoso-Júnior A, Coelho LG, Savassi-Rocha PR, et al. Gastric emptying of solids and semi-solids in morbidly obese and non-obese subjects: an assessment using the 13C-octanoic acid and 13C-acetic acid breath tests. Obes Surg. 2007. 17:236–241.51. Jackson SJ, Leahy FE, McGowan AA, Bluck LJ, Coward WA, Jebb SA. Delayed gastric emptying in the obese: an assessment using the non-invasive (13)C-octanoic acid breath test. Diabetes Obes Metab. 2004. 6:264–270.52. Cummings DE, Weigle DS, Frayo RS, et al. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med. 2002. 346:1623–1630.53. Hansen TK, Dall R, Hosoda H, et al. Weight loss increases circulating levels of ghrelin in human obesity. Clin Endocrinol (Oxf). 2002. 56:203–206.54. Lee KJ, Cha DY, Cheon SJ, Yeo M, Cho SW. Plasma ghrelin levels and their relationship with gastric emptying in patients with dysmotility-like functional dyspepsia. Digestion. 2009. 80:58–63.55. Cremonini F, Locke GR 3rd, Schleck CD, Zinsmeister AR, Talley NJ. Relationship between upper gastrointestinal symptoms and changes in body weight in a population-based cohort. Neurogastroenterol Motil. 2006. 18:987–994.56. Foster A, Laws HL, Gonzalez QH, Clements RH. Gastrointestinal symptomatic outcome after laparoscopic Roux-en-Y gastric bypass. J Gastrointest Surg. 2003. 7:750–753.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Obesity and Functional Gastrointestinal Disorders
- Pharmacological Treatment for FunctionalAbdominal Pain in Children
- Natural History and Overlap of Functional Gastrointestinal Disorders
- Validation of Rome III Criteria in the Diagnosis of Functional Gastrointestinal Disorders in Korean Patients
- Health Related Quality of Life in Functional Gastrointestinal Disorders in Asia