J Korean Surg Soc.
2010 Jan;78(1):58-61. 10.4174/jkss.2010.78.1.58.
Retroperitoneal Abscess in a Patient with Acute Appendicitis
- Affiliations
-
- 1Department of Surgery, Seoul National University Boramae Hospital, Seoul, Korea. kiterius@snu.ac.kr
- KMID: 1775447
- DOI: http://doi.org/10.4174/jkss.2010.78.1.58
Abstract
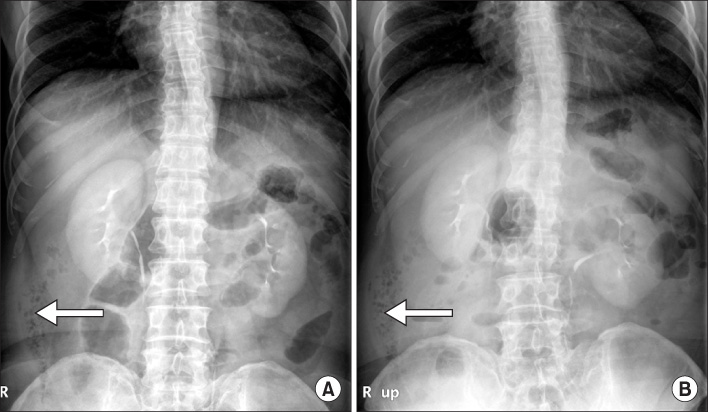
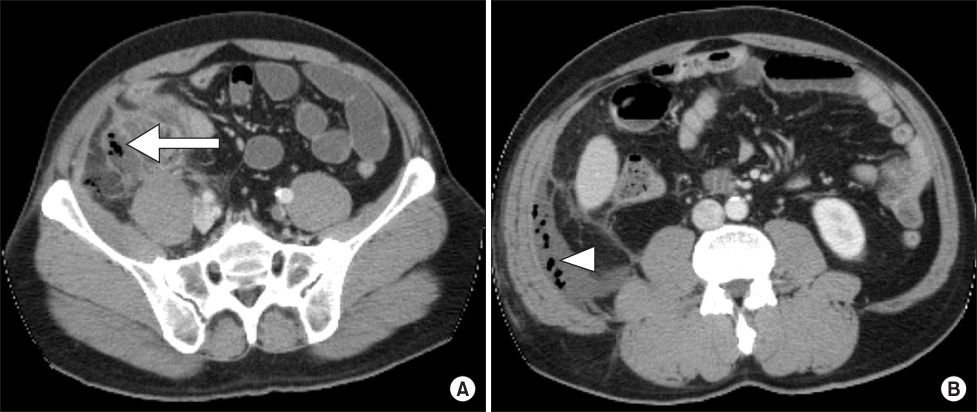
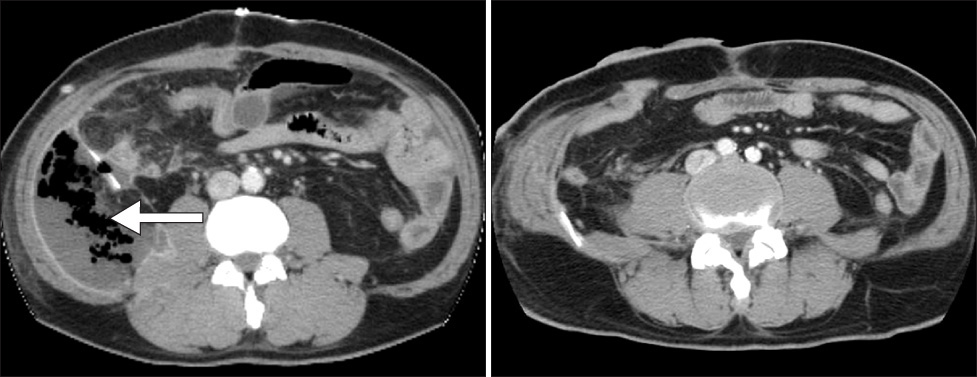
- Although acute appendicitis is one of the most common surgical diseases, very rare but serious complications can occur including retroperitoneal abscess complicated by acute appendicitis. The early diagnosis of retroperitoneal abscess is often difficult and delayed because its clinical course is often insidious and does not present with typical symptoms of acute appendicitis. We experienced a 65-year-old male patient who was diagnosed with acute appendicitis with retroperitoneal abscess. As the retroperitoneal abscess was not fully removed via emergency operation, postoperative percutaneous drainage was performed but not effective. Retroperitoneal abscess can be cured by 2nd operation with retroperitoneal approach. We report here an unusual case of retroperitoneal abscess complicated by acute appendicitis.
Figure
Reference
-
1. Lee SC, Lee BH. A clinical analysis of 2503 emergent explo-laparotomic cases. J Korean Surg Soc. 1999. 57:62–71.2. Crepps JT, Welch JP, Orlando R 3rd. Management and outcome of retroperitoneal abscesses. Ann Surg. 1987. 205:276–281.3. Blomqvist PG, Andersson RE, Granath F, Lambe MP, Ekbom AR. Mortality after appendectomy in Sweden, 1987-1996. Ann Surg. 2001. 233:455–460.4. Ko KH, Cho YP, Jung SM, Choi SJ, Kim SS, Jang HJ, et al. Necrotizing fasciitis secondary to perforated appendicitis. J Korean Surg Soc. 2004. 67:70–74.5. Ishikawa K. Retroperitoneal anatomy and pathology. Surgical Therapy. 2004. 90:807–814.6. Lambo A, Nchimi A, Khamis J, Khuc T. Retroperitoneal abscess from dropped appendicolith complicating laparoscopic appendectomy. Eur J Pediatr Surg. 2007. 17:139–141.7. Cho HJ, Whang IY, Kim JI, Ahn CH, Kim JS, Yoo SJ. The role of abdomen-pelvis CT for the diagnosis of appendicitis. J Korean Surg Soc. 2008. 75:90–95.8. Feldberg MA, Hendriks MJ, van Waes PF. Computed tomography in complicated acute appendicitis. Gastrointest Radiol. 1985. 10:289–295.9. Kaminski A, Liu IL, Applebaum H, Lee SL, Haigh PI. Routine interval appendectomy is not justified after initial nonoperative treatment of acute appendicitis. Arch Surg. 2005. 140:897–901.10. Hsieh CH, Wang YC, Yang HR, Chung PK, Jeng LB, Chen RJ. Retroperitoneal abscess resulting from perforated acute appendicitis: analysis of its management and outcome. Surg Today. 2007. 37:762–767.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Left Ureteral Obstruction due to Acute Appendicitis
- Endoscopic Drainage Through a Duodenal Fistula in a Patient with a Retroperitoneal Abscess that Developed after Acute Pancreatitis
- Antibiotic therapy for appendicitis treatment
- The Significance of Retroperitoneal Drainage for the Patients of Acute Infected Pancreatic Necrosis
- A Case of Pelvic Abscess Due to the Perforated Appendicitis