Korean Circ J.
2013 Feb;43(2):100-109. 10.4070/kcj.2013.43.2.100.
Effect of Early Statin Treatment in Patients with Cardiogenic Shock Complicating Acute Myocardial Infarction
- Affiliations
-
- 1Department of Cardiovascular Medicine, Chonnam National University College of Medicine, Gwangju, Korea. myungho@chollian.net
- 2Department of Cardiology, Yeungnam University College of Medicine, Daegu, Korea.
- 3Department of Cardiology, Kyungpuk National University College of Medicine, Daegu, Korea.
- 4Department of Cardiology, Busan National University College of Medicine, Busan, Korea.
- 5Department of Cardiology, Chungnam National University College of Medicine, Daejeon, Korea.
- 6Department of Cardiology, Chonbuk National University College of Medicine, Jeonju, Korea.
- 7Department of Cardiovascular Medicine, Kyung Hee University College of Medicine, Seoul, Korea.
- 8Department of Cardiology, Chungbuk National University College of Medicine, Cheongju, Korea.
- 9Department of Cardiology, Korea University College of Medicine, Guro Hospital, Seoul, Korea.
- 10Department of Cardiology, Konyang University College of Medicine, Daejeon, Korea.
- 11Department of Cardiovascular Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 12Department of Cardiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- KMID: 1769645
- DOI: http://doi.org/10.4070/kcj.2013.43.2.100
Abstract
- BACKGROUND AND OBJECTIVES
The benefit of early statin treatment following acute myocardial infarction (MI) complicated with cardiogenic shock (CS) has not been well studied. We sought to assess the effect of early statin therapy in patients with CS complicating acute MI.
SUBJECTS AND METHODS
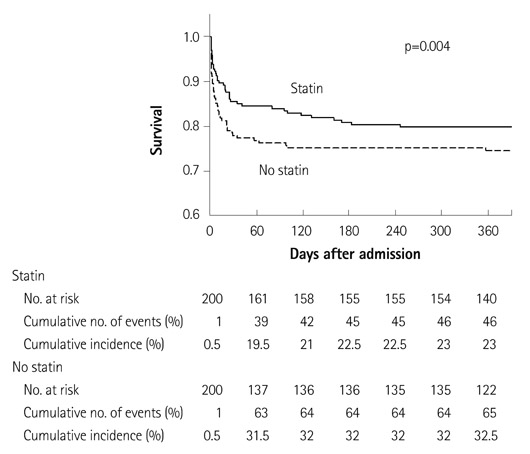
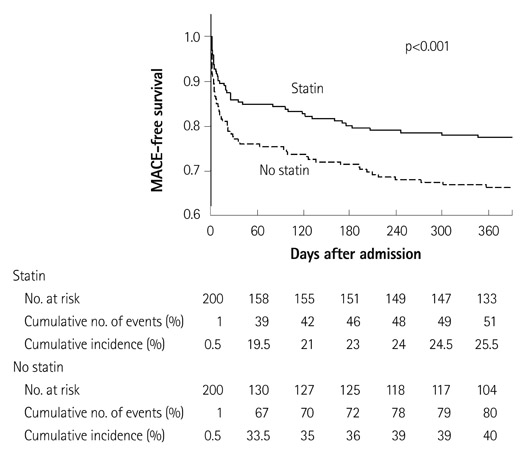
We studied 553 statin-naive patients with acute MI and CS (Killip class IV) who underwent revascularization therapy between November 2005 and January 2008 at 51 hospitals in the Korea Acute Myocardial Infarction Registry. Patients were divided into 2 groups: those who received statins during hospitalization (n=280) and those who did not (n=273). The influence of statin treatment on a 12-month clinical outcome was examined using a matched-pairs analysis (n=200 in each group) based on the propensity for receiving statin therapy during hospitalization.
RESULTS
Before adjustment, patients receiving statin, compared to those not receiving statin, had a more favorable clinical profile, were less likely to suffer procedural complications, and more likely to receive adequate medical therapy. Patients receiving statin had lower unadjusted in-hospital mortality and composite rate of mortality, MI, and repeat revascularization at 12 months, which remained significantly lower after adjustment for patient risk, procedural characteristics, and treatment propensity.
CONCLUSION
In CS patients with acute MI undergoing revascularization therapy, early statin treatment initiated during hospitalization was associated with lower rates of in-hospital death and 12-month adverse cardiac events.
Keyword
MeSH Terms
Figure
Reference
-
1. Krumholz HM, Anderson JL, Bachelder BL, et al. ACC/AHA 2008 performance measures for adults with ST-elevation and non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures (Writing Committee to develop performance measures for ST-elevation and non-ST-elevation myocardial infarction): developed in collaboration with the American Academy of Family Physicians and the American College of Emergency Physicians: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation, Society for Cardiovascular Angiography and Interventions, and Society of Hospital Medicine. Circulation. 2008. 118:2596–2648.2. Antman EM, Hand M, Armstrong PW, et al. 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee. Circulation. 2008. 117:296–329.3. Hamm CW, Bassand JP, Agewall S, et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: the Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2011. 32:2999–3054.4. Wright RS, Anderson JL, Adams CD, et al. 2011 ACCF/AHA Focused Update of the Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction (Updating the 2007 Guideline): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011. 123:2022–2060.5. Goldberg RJ, Spencer FA, Gore JM, Lessard D, Yarzebski J. Thirty-year trends (1975 to 2005) in the magnitude of, management of, and hospital death rates associated with cardiogenic shock in patients with acute myocardial infarction: a population-based perspective. Circulation. 2009. 119:1211–1219.6. TRIUMPH Investigators. Alexander JH, Reynolds HR, et al. Effect of tilarginine acetate in patients with acute myocardial infarction and cardiogenic shock: the TRIUMPH randomized controlled trial. JAMA. 2007. 297:1657–1666.7. Sim DS, Kim JH, Jeong MH. Differences in Clinical Outcomes Between Patients With ST-Elevation Versus Non-ST-Elevation Acute Myocardial Infarction in Korea. Korean Circ J. 2009. 39:297–303.8. Sim DS, Jeong MH, Kang JC. Current management of acute myocardial infarction: experience from the Korea Acute Myocardial Infarction Registry. J Cardiol. 2010. 56:1–7.9. D'Agostino RB Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998. 17:2265–2281.10. Joffe MM, Rosenbaum PR. Invited commentary: propensity scores. Am J Epidemiol. 1999. 150:327–333.11. Gu XS, Rosenbaum PR. Comparison of Multivariate Matching Methods: Structures, Distances, and Algorithms. J Comput Graph Stat. 1993. 2:405–420.12. Arntz HR, Agrawal R, Wunderlich W, et al. Beneficial effects of pravastatin (+/-colestyramine/niacin) initiated immediately after a coronary event (the randomized Lipid-Coronary Artery Disease [L-CAD] Study). Am J Cardiol. 2000. 86:1293–1298.13. Aronow HD, Novaro GM, Lauer MS, et al. In-hospital initiation of lipid-lowering therapy after coronary intervention as a predictor of longterm utilization: a propensity analysis. Arch Intern Med. 2003. 163:2576–2582.14. Fonarow GC, Wright RS, Spencer FA, et al. Effect of statin use within the first 24 hours of admission for acute myocardial infarction on early morbidity and mortality. Am J Cardiol. 2005. 96:611–616.15. Muhlestein JB, Horne BD, Bair TL, et al. Usefulness of in-hospital prescription of statin agents after angiographic diagnosis of coronary artery disease in improving continued compliance and reduced mortality. Am J Cardiol. 2001. 87:257–261.16. Li YH, Wu HL, Yang YH, Tsai HS, Chao TH. Effect of early versus late in-hospital initiation of statin therapy on the clinical outcomes of patients with acute coronary syndrome. Int Heart J. 2007. 48:677–688.17. Kim MC, Ahn Y, Cho KH, et al. Early statin therapy within 48 hours decreased one-year major adverse cardiac events in patients with acute myocardial infarction. Int Heart J. 2011. 52:1–6.18. Spencer FA, Allegrone J, Goldberg RJ, et al. Association of statin therapy with outcomes of acute coronary syndromes: the GRACE study. Ann Intern Med. 2004. 140:857–866.19. Garot P, Bendaoud N, Lefèvre T, Morice MC. Favourable effect of statin therapy on early survival benefit at the time of percutaneous coronary intervention for ST-elevation myocardial infarction and shock. EuroIntervention. 2010. 6:350–355.20. Schmidt H, Hennen R, Keller A, et al. Association of statin therapy and increased survival in patients with multiple organ dysfunction syndrome. Intensive Care Med. 2006. 32:1248–1251.21. Pruefer D, Makowski J, Schnell M, et al. Simvastatin inhibits inflammatory properties of Staphylococcus aureus alpha-toxin. Circulation. 2002. 106:2104–2110.22. Tracey KJ. The inflammatory reflex. Nature. 2002. 420:853–859.23. Schmidt H, Müller-Werdan U, Hoffmann T, et al. Autonomic dysfunction predicts mortality in patients with multiple organ dysfunction syndrome of different age groups. Crit Care Med. 2005. 33:1994–2002.24. Schmidt H, Hoyer D, Hennen R, et al. Autonomic dysfunction predicts both 1- and 2-month mortality in middle-aged patients with multiple organ dysfunction syndrome. Crit Care Med. 2008. 36:967–970.25. Merx MW, Liehn EA, Janssens U, et al. HMG-CoA reductase inhibitor simvastatin profoundly improves survival in a murine model of sepsis. Circulation. 2004. 109:2560–2565.26. Merx MW, Liehn EA, Graf J, et al. Statin treatment after onset of sepsis in a murine model improves survival. Circulation. 2005. 112:117–124.27. Almog Y, Shefer A, Novack V, et al. Prior statin therapy is associated with a decreased rate of severe sepsis. Circulation. 2004. 110:880–885.28. Hackam DG, Mamdani M, Li P, Redelmeier DA. Statins and sepsis in patients with cardiovascular disease: a population-based cohort analysis. Lancet. 2006. 367:413–418.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Percutaneous Transluminal Coronary Angioplasty in Treatment of Cardiogenic Shock Complicating Acute Myocardial Infarction
- The Effect of Early IABP and Reperfusion therapy in Patient of Post MI Cardiogenic shock
- Mechanical Circulatory Support in the Cardiac Catheterization Laboratory for Cardiogenic Shock
- Coronary Intervention of Cardiogenic Shock in Acute Myocardial Infarction
- A Case of COVID-19 with Acute Myocardial Infarction and Cardiogenic Shock