Yonsei Med J.
2009 Jun;50(3):385-390. 10.3349/ymj.2009.50.3.385.
Development of New Cardiac Deformity Indexes for Pectus Excavatum on Computed Tomography: Feasibility for Pre- and Post-Operative Evaluation
- Affiliations
-
- 1Department of Diagnostic Radiology, Korea University Hospital, Ansan, Korea. kiylee@korea.ac.kr
- 2Department of Thoracic Surgery, Korea University Hospital, Ansan, Korea.
- 3Department of Biostatistics, Korea University Hospital, Ansan, Korea.
- KMID: 1758567
- DOI: http://doi.org/10.3349/ymj.2009.50.3.385
Abstract
-
PURPOSE: The aim of this study was to evaluate new cardiac deformity indexes (CDIs) for diagnosis of pectus excavatum as well as morphological assessment of heart on computed tomography (CT).
MATERIALS AND METHODS
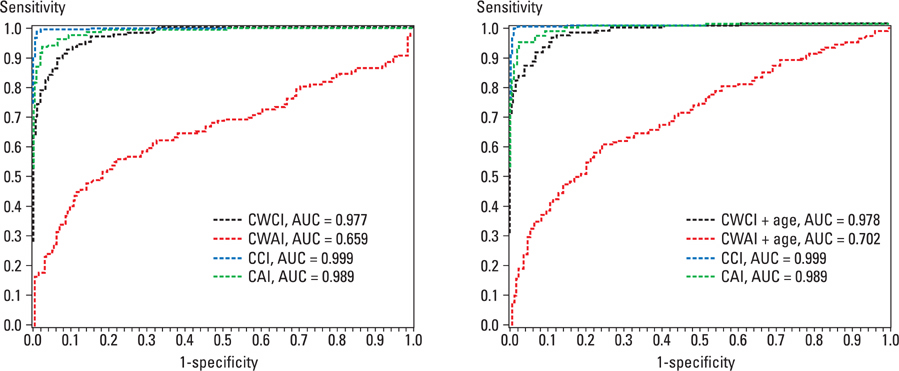
We retrospectively evaluated the CT images of the control group (n=200), and the pectus excavatum before and after correction groups (n=178), and calculated the CDIs; cardiac compression index (CCI), and cardiac asymmetry index (CAI). We also calculated chest wall compression index (CWCI) and asymmetry index (CWAI) on the axial images. We performed logistic regression analysis using each index and age as predictor variables.
RESULTS
The CDIs (CCI and CAI) were significant (p < 0.05) in the diagnosis of pectus excavatum, regardless of age (p = 0.4033, p = 0.8113). The CWCI and CWAI were significant (p < 0.05) and significantly affected by age (p < 0.05). If we selected 1.82 as the cutoff of the CCI, the sensitivity and specificity were 99.4% and 98%, respectively. The following cutoffs and the sensitivity and specificity were obtained: 1.15 for the CAI gave 94.4% and 94.5%, 3.05 for the CWCI gave 92.1% and 92%, and 1 for the CWAI gave 62.4% and 65%, respectively. The CCI after repair improved from 2.83 +/- 0.84 to 1.84 +/- 0.33, while the CWCI improved from 4.49 +/- 1.61 to 2.57 +/- 0.44.
CONCLUSION
CDIs such as the CCI and CAI may be potentially useful to detect and estimate repair for pectus excavatum.
Keyword
MeSH Terms
Figure
Reference
-
1. Guller B, Hable K. Cardiac findings in pectus excavatum in children: review and differential diagnosis. Chest. 1974. 66:165–171.
Article2. Wachtel FW, Ravitch MM, Grishman A. The relation of pectus excavatum to heart disease. Am Heart J. 1956. 52:121–137.3. Nuss D, Kelly RE Jr, Croitoru DP, Katz ME. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg. 1998. 33:545–552.4. Park HJ, Lee SY, Lee CS, Youm W, Lee KR. The Nuss procedure for pectus excavatum: evolution of techniques and early results on 322 patients. Ann Thorac Surg. 2004. 77:289–295.
Article5. Park HJ, Lee SY, Lee CS. Complications associated with the Nuss procedure: analysis of risk factors and suggested measures for prevention of complications. J Pediatr Surg. 2004. 39:391–395.
Article6. Park HJ. Technical Innovations in minimally invasive approach for pectus excavatum: a paradigm shift through 630 patients. Innovations. 2007. 2:25–28.
Article7. Sigalet DL, Montgomery M, Harder J. Cardiopulmonary effects of closed repair of pectus excavatum. J Pediatr Surg. 2003. 38:380–385.
Article8. Borowitz D, Cerny F, Zallen G, Sharp J, Burke M, Gross K, et al. Pulmonary function and exercise response in patients with pectus excavatum after Nuss repair. J Pediatr Surg. 2003. 38:544–547.
Article9. Bawazir OA, Montgomery M, Harder J, Sigalet DL. Midterm evaluation of cardiopulmonary effects of closed repair for pectus excavatum. J Pediatr Surg. 2005. 40:863–867.
Article10. Coln E, Carrasco J, Coln D. Demonstrating relief of cardiac compression with the Nuss minimally invasive repair for pectus excavatum. J Pediatr Surg. 2006. 41:683–686.
Article11. Nakagawa Y, Uemura S, Nakaoka T, Yano T, Tanaka N. Evaluation of the Nuss procedure using pre-and postoperative computed tomographic index. J Pediatr Surg. 2008. 43:518–521.
Article12. Haller JA Jr, Kramer SS, Lietman SA. Use of CT scans in selection of patients for pectus excavatum surgery: a preliminary report. J Pediatr Surg. 1987. 22:904–906.
Article13. Kim HC, Park HJ, Ham SY, Nam KW, Choi SY, Oh JS, et al. Development of automatized new indices for radiological assessment of chest-wall deformity and its quantitative evaluation. Med Biol Eng Comput. 2008. 46:815–823.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Repair of Recurrent Pectus Excavatum with a Huge Chest Wall Defect in a Patient with a Previous Ravitch and Pectus Bar Repair: A Case Report
- Cardiac Cachexia Caused by Right Ventricular Outflow Tract Obstruction in a Patient With Severe Pectus Excavatum
- Embarrassed Radiofrequency Catheter Ablation of Supraventricular Tachycardia in Pectus Excavatum
- Cardiac Arrest during the Rotation of a Stainless Steel Bar in a Patient undergoing the Pectus Excavatum Repair : A case report
- Combined Repair of Pectus Excavatum and Open Heart Surgery in Marfan's Syndrome