Korean J Lab Med.
2011 Jul;31(3):143-147. 10.3343/kjlm.2011.31.3.143.
Evaluation of the Diagnostic Performance of Fibrin Monomer in Disseminated Intravascular Coagulation
- Affiliations
-
- 1Department of Laboratory Medicine & Genetics, Samsung Medical Center, Sungkyunkwan University School Medicine, Seoul, Korea. heejinkim@skku.edu
- KMID: 1735844
- DOI: http://doi.org/10.3343/kjlm.2011.31.3.143
Abstract
- BACKGROUND
Fibrin-related markers (FRM) such as fibrin monomer (FM) and D-dimer (DD) are considered useful biological markers for the diagnosis of disseminated intravascular coagulation (DIC). However, no studies on the diagnostic performance of different FRMs have been published in Korea. The aim of this study was to evaluate the diagnostic performance of FM for DIC in comparison with DD.
METHODS
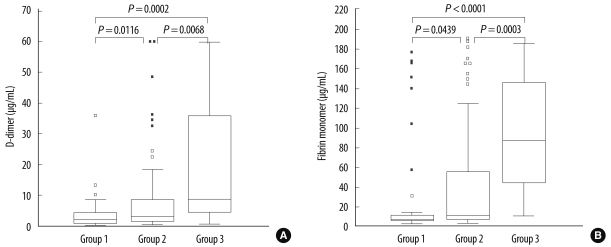
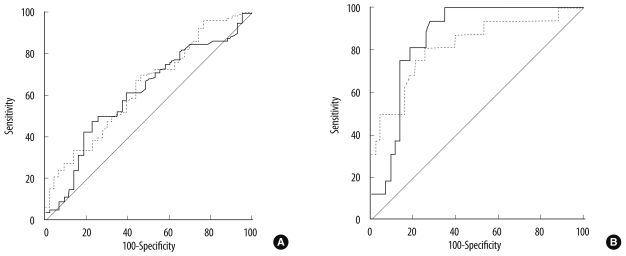
The reference limit of FM was determined based on plasma sample data obtained from 210 control individuals. To evaluate diagnostic performance, FM data from the plasma samples of 139 patients with DIC-associated diseases were obtained for DIC scoring. FM was measured by immunoturbidimetry using STA-LIATEST FM (Diagnostica Stago, France). Patients were classified according to the DIC score as non-DIC, non-overt DIC, or overt DIC. ROC curve analyses were performed.
RESULTS
The reference limit in the control individuals was determined to be 7.80 microg/mL. Patients with DIC-associated diseases were categorized as non-DIC (N=43), non-overt DIC (N=80), and overt DIC (N=16). ROC curve analyses showed that the diagnostic performance of FM was comparable to DD in both non-overt DIC and overt DIC (P=0.596 and 0.553, respectively). In addition, FM had higher sensitivity, specificity, positive predictive value, and negative predictive value than DD for differentiating overt DIC from non-DIC.
CONCLUSIONS
This study demonstrated that the diagnostic performance of FM for DIC was comparable to DD. FM might be more sensitive and more specific than DD in the diagnosis of overt DIC, but not non-overt DIC.
Keyword
MeSH Terms
Figure
Reference
-
1. Levi M, Toh CH, Thachil J, Watson HG. British Committee for Standards in Haematology. Guidelines for the diagnosis and management of disseminated intravascular coagulation. Br J Haematol. 2009; 145:24–33. PMID: 19222477.
Article2. Toh CH, Hoots WK. The scoring system of the Scientific and Standardisation Committee on Disseminated Intravascular Coagulation of the International Society on Thrombosis and Haemostasis: a 5-year overview. J Thromb Haemost. 2007; 5:604–606. PMID: 17096704.
Article3. Taylor FB Jr, Toh CH, Hoots WK, Wada H, Levi M. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001; 86:1327–1330. PMID: 11816725.
Article4. Wada H, Sakuragawa N. Are fibrin-related markers useful for the diagnosis of thrombosis? Semin Thromb Hemost. 2008; 34:33–38. PMID: 18393141.
Article5. Wada H, Sase T, Matsumoto T, Kushiya F, Sakakura M, Mori Y, et al. Increased soluble fibrin in plasma of patients with disseminated intravascular coagulation. Clin Appl Thromb Hemost. 2003; 9:233–240. PMID: 14507112.
Article6. Dempfle CE, Wurst M, Smolinski M, Lorenz S, Osika A, Olenik D, et al. Use of soluble fibrin antigen instead of D-dimer as fibrin-related marker may enhance the prognostic power of the ISTH overt DIC score. Thromb Haemost. 2004; 91:812–818. PMID: 15045145.
Article7. Ieko M, Nakabayashi T, Tarumi T, Naito S, Yoshida M, Kanazawa K, et al. Soluble fibrin monomer degradation products as a potentially useful marker for hypercoagulable states with accelerated fibrinolysis. Clin Chim Acta. 2007; 386:38–45. PMID: 17803984.
Article8. Wada H, Wakita Y, Nakase T, Shimura M, Hiyoyama K, Nagaya S, et al. Increased plasma-soluble fibrin monomer levels in patients with disseminated intravascular coagulation. Am J Hematol. 1996; 51:255–260. PMID: 8602623.
Article9. Toh CH, Downey C. Performance and prognostic importance of a new clinical and laboratory scoring system for identifying non-overt disseminated intravascular coagulation. Blood Coagul Fibrinolysis. 2005; 16:69–74. PMID: 15650549.
Article10. Okajima K, Uchiba M, Murakami K, Okabe H, Takatsuki K. Determination of plasma soluble fibrin using a new ELISA method in patients with disseminated intravascular coagulation. Am J Hematol. 1996; 51:186–191. PMID: 8619398.
Article11. Hamano A, Umeda M, Ueno Y, Tanaka S, Mimuro J, Sakata Y. Latex immunoturbidimetric assay for soluble fibrin complex. Clin Chem. 2005; 51:183–188. PMID: 15514091.
Article12. Okamoto K, Wada H, Hatada T, Uchiyama T, Kawasugi K, Mayumi T, et al. Frequency and hemostatic abnormalities in pre-DIC patients. Thromb Res. 2010; 126:74–78. PMID: 20452653.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnostic Utility of D-dimer Test in Disseminated Intravascular Coagulation with Sepsis
- Disseminated intravascular coagulation due to placenta accreta : A case report
- Postoperative Severe Hemorrhage Due to Disseminated Intravascular Coagulation: A case report
- Diagnostic efficacy of fibrinogen degradation product(FgDP) assay in disseminated intravascular coagulation
- Diagnostic efficacy of plasma D-dimer assay in evaluating disseminated intravascular coagulation: comparison with serum FDP assay based on ROC method