Yonsei Med J.
2012 Jul;53(4):788-793. 10.3349/ymj.2012.53.4.788.
Transdermal Fentanyl for Chronic Low Back Pain
- Affiliations
-
- 1Department of Orthopaedic Surgery, Graduate School of Medicine, Chiba University, Chiba, Japan. sohtori@faculty.chiba-u.jp
- KMID: 1716879
- DOI: http://doi.org/10.3349/ymj.2012.53.4.788
Abstract
- PURPOSE
Chronic low back pain is a common clinical problem. As medication, non-steroidal anti-inflammatory drugs are generally used; however, they are sometimes non-effective. Recently, opioids have been used for the treatment of chronic low back pain, and since 2010, transdermal fentanyl has been used to treat chronic non-cancer pain in Japan. The purpose of the current study was to examine the efficacy of transdermal fentanyl in the treatment of chronic low back pain.
MATERIALS AND METHODS
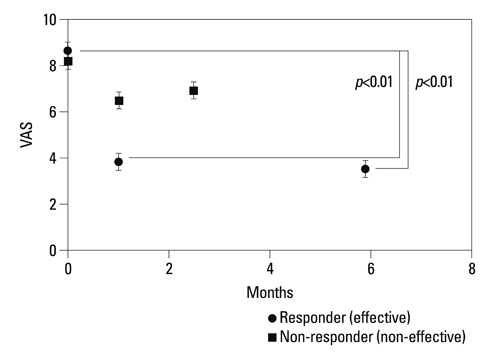
This study included patients (n=62) that suffered from chronic low back pain and were non-responsive to non-steroidal anti-inflammatory drugs. Their conditions consisted of non-specific low back pain, multiple back operations, and specific low back pain awaiting surgery. Patients were given transdermal fentanyl for chronic low back pain. Scores of the visual analogue scale and the Oswestry Disability Index, as well as adverse events were evaluated before and after therapy.
RESULTS
Overall, visual analogue scale scores and Oswestry Disability Index scores improved significantly after treatment. Transdermal fentanyl (12.5 to 50 microg/h) was effective in reducing low back pain in 45 of 62 patients; however, it was not effective in 17 patients. Patients who experienced the most improvement were those with specific low back pain awaiting surgery. Adverse events were seen in 40% of patients (constipation, 29%; nausea, 24%; itching, 24%).
CONCLUSION
Disability Index scores in 73% of patients, especially those with specific low back pain awaiting surgery; however, it did not decrease pain in 27% of patients, including patients with non-specific low back pain or multiple back operations.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Regulatory Role of Hypoxia Inducible Factor in the Biological Behavior of Nucleus Pulposus Cells
Hao Li, Cheng Zhen Liang, Qi Xin Chen
Yonsei Med J. 2013;54(4):807-812. doi: 10.3349/ymj.2013.54.4.807.
Reference
-
1. Mirza SK, Deyo RA. Systematic review of randomized trials comparing lumbar fusion surgery to nonoperative care for treatment of chronic back pain. Spine (Phila Pa 1976). 2007. 32:816–823.
Article2. Ohtori S, Koshi T, Yamashita M, Yamauchi K, Inoue G, Suzuki M, et al. Surgical versus nonsurgical treatment of selected patients with discogenic low back pain: a small-sized randomized trial. Spine (Phila Pa 1976). 2011. 36:347–354.
Article3. Wolfe MM, Lichtenstein DR, Singh G. Gastrointestinal toxicity of nonsteroidal antiinflammatory drugs. N Engl J Med. 1999. 340:1888–1899.
Article4. McQuay H. Opioids in pain management. Lancet. 1999. 353:2229–2232.
Article5. McNairy SL, Maruta T, Ivnik RJ, Swanson DW, Ilstrup DM. Prescription medication dependence and neuropsychologic function. Pain. 1984. 18:169–177.
Article6. Allan L, Hays H, Jensen NH, de Waroux BL, Bolt M, Donald R, et al. Randomised crossover trial of transdermal fentanyl and sustained release oral morphine for treating chronic non-cancer pain. BMJ. 2001. 322:1154–1158.7. Franco ML, Seoane A. Usefulness of transdermal fentanyl in the management of nonmalignant chronic pain: a prospective, observational, multicenter study. Pain Clinic. 2002. 14:99–112.
Article8. Jeal W, Benfield P. Transdermal fentanyl. A review of its pharmacological properties and therapeutic efficacy in pain control. Drugs. 1997. 53:109–138.9. Adams LL, Gatchel RJ, Robinson RC, Polatin P, Gajraj N, Deschner M, et al. Development of a self-report screening instrument for assessing potential opioid medication misuse in chronic pain patients. J Pain Symptom Manage. 2004. 27:440–459.
Article10. Schnitzer TJ, Gray WL, Paster RZ, Kamin M. Efficacy of tramadol in treatment of chronic low back pain. J Rheumatol. 2000. 27:772–778.11. Ruoff GE, Rosenthal N, Jordan D, Karim R, Kamin M. Protocol CAPSS-112 Study Group. Tramadol/acetaminophen combination tablets for the treatment of chronic lower back pain: a multicenter, randomized, double-blind, placebo-controlled outpatient study. Clin Ther. 2003. 25:1123–1141.
Article12. Peloso PM, Fortin L, Beaulieu A, Kamin M, Rosenthal N. Protocol TRP-CAN-1 Study Group. Analgesic efficacy and safety of tramadol/acetaminophen combination tablets (Ultracet) in treatment of chronic low back pain: a multicenter, outpatient, randomized, double blind, placebo controlled trial. J Rheumatol. 2004. 31:2454–2463.13. Allan L, Richarz U, Simpson K, Slappendel R. Transdermal fentanyl versus sustained release oral morphine in strong-opioid naïve patients with chronic low back pain. Spine (Phila Pa 1976). 2005. 30:2484–2490.
Article14. Kosinski MR, Schein JR, Vallow SM, Ascher S, Harte C, Shikiar R, et al. An observational study of health-related quality of life and pain outcomes in chronic low back pain patients treated with fentanyl transdermal system. Curr Med Res Opin. 2005. 21:849–862.
Article15. Kalso E, Simpson KH, Slappendel R, Dejonckheere J, Richarz U. Predicting long-term response to strong opioids in patients with low back pain: findings from a randomized, controlled trial of transdermal fentanyl and morphine. BMC Med. 2007. 5:39.
Article16. Kalso E, Edwards JE, Moore RA, McQuay HJ. Opioids in chronic non-cancer pain: systematic review of efficacy and safety. Pain. 2004. 112:372–380.
Article17. Martell BA, O'Connor PG, Kerns RD, Becker WC, Morales KH, Kosten TR, et al. Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med. 2007. 146:116–127.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Fentanyl Intoxication Through Overusing Fentanyl Patch
- Clinical Usefulness of Fentanyl Matrix Patch for the Patients with Chronic Low Back Pain
- A Case of Fentanyl Toxicity with Misused Durogesic Transdermal Patch
- The Effectiveness of Transdermal Fentanyl Patch in Cancer Pain Patients
- Oceupational Chronic Low Baek Pain: A Case Report