Yonsei Med J.
2012 Jul;53(4):753-758. 10.3349/ymj.2012.53.4.753.
Clinical Features of Fitz-Hugh-Curtis Syndrome in the Emergency Department
- Affiliations
-
- 1Department of Emergency Medicine, Yonsei University College of Medicine, Seoul, Korea. Incheol@yuhs.ac
- 2Department of Diagnostic Radiology, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1716874
- DOI: http://doi.org/10.3349/ymj.2012.53.4.753
Abstract
- PURPOSE
Fitz-Hugh-Curtis Syndrome (FHCS) is a clinical entity characterized by inflammation of the liver capsule associated with genital tract infection. The aim of this study is to provide physicians with clinical suggestions for diagnostic approaches based on a series of patients who were diagnosed with FHCS.
MATERIALS AND METHODS
We conducted a retrospective study of patients who were diagnosed with FHCS after presenting to the emergency department (ED). The symptoms, physical examinations, laboratory findings, radiological findings, and progress of the patients were reviewed.
RESULTS
During the four-year study period, a total of 82 female patients received a final diagnosis of FHCS in the ED. Chlamydia trachomatis was identified as a pathogen in 89% of the patients. Their clinical characteristics and laboratory findings were described. Fifty-two patients (63.4%) were admitted to the hospital. All of the admitted patients improved after treatment combining antibiotic therapy with conservative care.
CONCLUSION
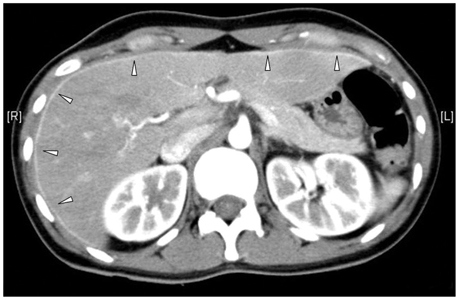
FHCS should be considered as a differential diagnosis for female patients of childbearing age with right upper abdominal pain. Timely diagnosis using biphasic computed tomography (CT) with arterial and portal phases may help ensure adequate medical treatment as well as avoid invasive procedures.
MeSH Terms
-
Adolescent
Adult
Anti-Bacterial Agents/therapeutic use
Chlamydia Infections/drug therapy/microbiology/*pathology/radiography
Chlamydia trachomatis/pathogenicity
Emergency Service, Hospital
Female
Hepatitis/drug therapy/microbiology/*pathology/radiography
Humans
Pelvic Inflammatory Disease/drug therapy/microbiology/*pathology/radiography
Peritonitis/drug therapy/microbiology/*pathology/radiography
Reproductive Tract Infections/drug therapy/microbiology/pathology/radiography
Retrospective Studies
Tomography, X-Ray Computed
Young Adult
Figure
Reference
-
1. Curtis AH. A cause of adhesions in the right upper quadrant. J Am Med Assoc. 1930. 94:1221–1222.
Article2. Fitz-Hugh T Jr. Acute gonococcic peritonitis of the right upper quadrant in women. J Am Med Assoc. 1934. 102:2094–2096.
Article3. Wølner-Hanssen P, Svensson L, Weström L, Märdh PA. Isolation of Chlamydia trachomatis from the liver capsule in Fitz-Hugh-Curtis syndrome. N Engl J Med. 1982. 306:113.
Article4. Nishie A, Yoshimitsu K, Irie H, Yoshitake T, Aibe H, Tajima T, et al. Fitz-Hugh-Curtis syndrome. Radiologic manifestation. J Comput Assist Tomogr. 2003. 27:786–791.5. McCormick M, DelCastillo J, Berk RS. An atypical presentation of the Fitz-Hugh-Curtis syndrome. J Emerg Med. 1990. 8:55–58.
Article6. Counselman FL. An unusual presentation of Fitz-Hugh-Curtis syndrome. J Emerg Med. 1994. 12:167–170.
Article7. Tsubuku M, Hayashi S, Terahara A, Furukawa T, Ohmura G. Fitz-Hugh-Curtis syndrome: linear contrast enhancement of the surface of the liver on CT. J Comput Assist Tomogr. 2002. 26:456–458.
Article8. Joo SH, Kim MJ, Lim JS, Kim JH, Kim KW. CT diagnosis of Fitz-Hugh and Curtis syndrome: value of the arterial phase scan. Korean J Radiol. 2007. 8:40–47.
Article9. Kim JY, Kim Y, Jeong WK, Song SY, Cho OK. Perihepatitis with pelvic inflammatory disease (PID) on MDCT: characteristic findings and relevance to PID. Abdom Imaging. 2009. 34:737–742.
Article10. Peter NG, Clark LR, Jaeger JR. Fitz-Hugh-Curtis syndrome: a diagnosis to consider in women with right upper quadrant pain. Cleve Clin J Med. 2004. 71:233–239.
Article11. Kimball MW, Knee S. Gonococcal perihepatitis in a male. The Fitz-Hugh--Curtis syndrome. N Engl J Med. 1970. 282:1082–1084.12. Choi TY, Kang JO, Chung SR, Ahn Y. [Chlamydia trachomatis antibody in Fitz-Hugh-Curtis syndrome]. Korean J Lab Med. 2008. 28:293–298.13. Zeger W, Holt K. Gynecologic infections. Emerg Med Clin North Am. 2003. 21:631–648.
Article14. Gatt D, Jantet G. Perisplenitis and perinephritis in the Curtis-Fitz-Hugh syndrome. Br J Surg. 1987. 74:110–112.
Article15. Ris HW. Perihepatitis (Fitz-Hugh--Curtis syndrome). A review and case presentation. J Adolesc Health Care. 1984. 5:272–276.16. Woo SY, Kim JI, Cheung DY, Cho SH, Park SH, Han JY, et al. Clinical outcome of Fitz-Hugh-Curtis syndrome mimicking acute biliary disease. World J Gastroenterol. 2008. 14:6975–6980.
Article17. Sharma JB, Roy KK, Gupta N, Jain SK, Malhotra N, Mittal S. High prevalence of Fitz-Hugh-Curtis Syndrome in genital tuberculosis. Int J Gynaecol Obstet. 2007. 99:62–63.
Article18. Gandhi SG, Komenaka IK, Naim JH. Fitz-Hugh-Curtis syndrome after laparoscopic tubal ligation. A case report. J Reprod Med. 2003. 48:302–305.19. Wang CL, Guo XJ, Yuan ZD, Shi Q, Hu XH, Fang L. Radiologic diagnosis of Fitz-Hugh-Curtis syndrome. Chin Med J (Engl). 2009. 122:741–744.20. Kim S, Kim TU, Lee JW, Lee TH, Lee SH, Jeon TY, et al. The perihepatic space: comprehensive anatomy and CT features of pathologic conditions. Radiographics. 2007. 27:129–143.
Article21. Schoenwaelder M, Stuckey SL. Perihepatitis associated with systemic lupus erythematosus: computed tomography findings. Australas Radiol. 2005. 49:179–181.
Article22. Dinerman LM, Elfenbein DS, Cumming WA. Clinical Fitz-Hugh-Curtis syndrome in an adolescent. Ultrasonographic findings. Clin Pediatr (Phila). 1990. 29:532–535.23. Yang HW, Jung SH, Han HY, Kim A, Lee YJ, Cha SW, et al. [Clinical feature of Fitz-Hugh-Curtis syndrome: analysis of 25 cases]. Korean J Hepatol. 2008. 14:178–184.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Fitz-Hugh-Curtis syndrome in a male patient
- A case of Fitz-Hugh-Curtis syndrome diagnosed by pelvic CT imaging prior to diagnostic laparoscopy
- Inflammatory Pseudotumor in the Liver and Right Omentum Caused by Pelvic Inflammatory Disease: A Case Report
- Two Cases of Fitz - Hugh - Curtis Syndrome Associated with Ectopic Pregnancy
- A Case of Fitz-Hugh-Curtis Syndrome