Comorbidities of Chronic Obstructive Pulmonary Disease in Koreans: A Population-Based Study
- Affiliations
-
- 1Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. ymoh55@amc.seoul.kr
- 2Department of Pulmonary and Critical Care Medicine, Wonkwang University Sanbon Hospital, Gunpo, Korea.
- 3Clinical Research Center for Chronic Obstructive Airway Disease, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 1714202
- DOI: http://doi.org/10.3346/jkms.2012.27.8.901
Abstract
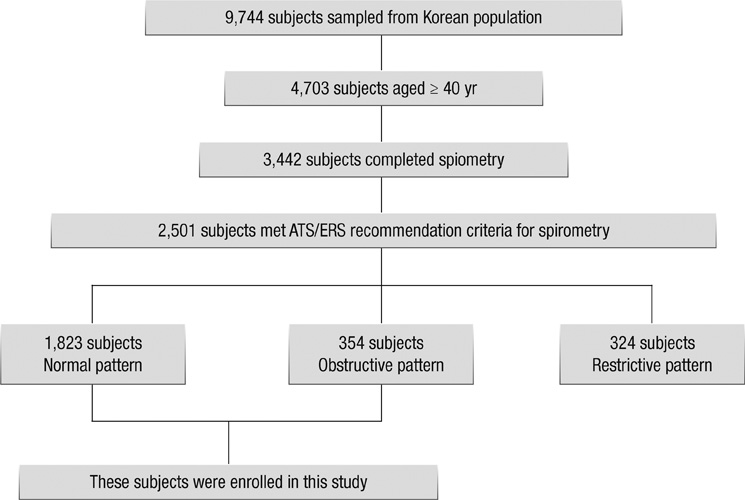
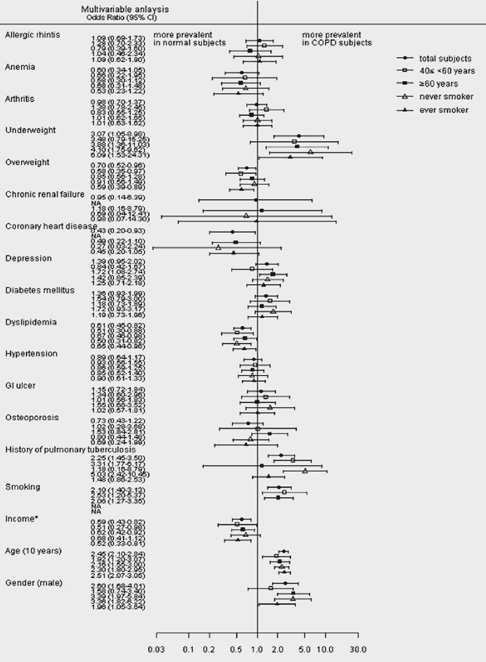
- Chronic obstructive pulmonary disease (COPD) includes pulmonary components with increased comorbidity rates, as well as being a systemic disease. Comorbidities may frequently occur in COPD patients over 40 yr old. We report the comorbidities of patients with COPD, diagnosed by spirometry, in a population-based epidemiologic survey in Korea. Data were derived from the fourth Korean Health and Nutrition Examination Survey in 2008, a stratified multistage clustered probability design survey of a sample representing the entire population of Korea. Results of spirometry and various health-related questionnaires were analyzed in 2,177 subjects aged > or = 40 yr. The prevalence of COPD (FEV1/FVC < 0.7) in subjects > or = 40 yr of age was 14.1%. Multivariate analysis showed that underweight (odds ratio [OR] 3.07, 95% confidence interval [CI] 1.05-8.98), coronary heart disease (OR, 0.43; 95% CI, 0.20-0.93) and dyslipidemia (OR, 0.61; 95% CI, 0.45-0.82) were significantly associated with COPD, whereas allergic rhinitis, anemia, arthritis, chronic renal failure, depression, diabetes mellitus, hypertension, gastrointestinal ulcer, and osteoporosis were not. Underweight might be more prevalent but coronary heart disease and dyslipidemia are less prevalent in Koreans with than without COPD in population setting.
MeSH Terms
Figure
Cited by 4 articles
-
Clinical Phenotypes, Comorbidities, and Exacerbations according to Serum 25-OH Vitamin D and Plasma Fibrinogen Levels in Chronic Obstructive Pulmonary Disease
Dong-gon Hyun, Yeon-mok Oh, Sei Won Lee, Sang Do Lee, Jae Seung Lee
J Korean Med Sci. 2019;34(29):. doi: 10.3346/jkms.2019.34.e195.The diagnosis of chronic obstructive pulmonary disease according to current guidelines
Hyun Jung Kim, Yeon-Mok Oh
J Korean Med Assoc. 2018;61(9):539-544. doi: 10.5124/jkma.2018.61.9.539.Word Embedding Reveals Cyfra 21-1 as a Biomarker for Chronic Obstructive Pulmonary Disease
Jeongwon Heo, Da Hye Moon, Yoonki Hong, So Hyeon Bak, Jeeyoung Kim, Joo Hyun Park, Byoung-Doo Oh, Yu-Seop Kim, Woo Jin Kim
J Korean Med Sci. 2021;36(35):e224. doi: 10.3346/jkms.2021.36.e224.Relationships Between Pulmonary Function and Composite Indices of Femoral Neck Strength in Korean Men (KNHANES IV)
Mihye Jung, Seong Hee Ahn, Seongha Seo, Yongin Cho, Da Hea Seo, So Hun Kim, Seongbin Hong
J Korean Med Sci. 2022;37(8):e66. doi: 10.3346/jkms.2022.37.e66.
Reference
-
1. Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997. 349:1269–1276.2. Fabbri LM, Rabe KF. From COPD to chronic systemic inflammatory syndrome? Lancet. 2007. 370:797–799.3. Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001. 163:1256–1276.4. Yoo JW, Hong Y, Seo JB, Chae EJ, Ra SW, Lee JH, Kim EK, Baek S, Kim TH, Kim WJ, et al. Comparison of clinico-physiologic and CT imaging risk factors for COPD exacerbation. J Korean Med Sci. 2011. 26:1606–1612.5. Hwang YI, Yoo KH, Sheen SS, Park JH, Kim SH, Yoon HI, Lim SC, Lee SY, Park JY, Park SJ. Prevalence of chronic obstructive pulmonary disease in Korea: the reasult of fourth Korean National Health and Nutrition Examination Survey. Tuberc Respir Dis. 2011. 71:328–334.6. Buist AS, McBurnie MA, Vollmer WM, Gillespie S, Burney P, Mannino DM, Menezes AM, Sullivan SD, Lee TA, Weiss KB, et al. International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet. 2007. 370:741–750.7. Tan WC, Ng TP. COPD in Asia: where East meets West. Chest. 2008. 133:517–527.8. Sin DD, Man SF. Why are patients with chronic obstructive pulmonary disease at increased risk of cardiovascular diseases? The potential role of systemic inflammation in chronic obstructive pulmonary disease. Circulation. 2003. 107:1514–1519.9. McGarvey LP, John M, Anderson JA, Zvarich M, Wise RA. Ascertainment of cause-specific mortality in COPD: operations of the TORCH Clinical Endpoint Committee. Thorax. 2007. 62:411–415.10. Izquierdo JL, Martinez A, Guzman E, de Lucas P, Rodriguez JM. Lack of association of ischemic heart disease with COPD when taking into account classical cardiovascular risk factors. Int J Chron Obstruct Pulmon Dis. 2010. 5:387–394.11. Lu M, Yao WZ, Zhong NS, Zhou YM, Wang C, Chen P, Kang J, Huang SG, Chen BY, Wang CZ, et al. Asymptomatic patients of chronic obstructive pulmonary disease in China. Chin Med J (Engl). 2010. 123:1494–1499.12. Nussbaumer-Ochsner Y, Rabe KF. Systemic manifestations of COPD. Chest. 2011. 139:165–173.13. Sidney S, Sorel M, Quesenberry CP Jr, DeLuise C, Lanes S, Eisner MD. COPD and incident cardiovascular disease hospitalizations and mortality: Kaiser Permanente Medical Care Program. Chest. 2005. 128:2068–2075.14. Curkendall SM, DeLuise C, Jones JK, Lanes S, Stang MR, Goehring E Jr, She D. Cardiovascular disease in patients with chronic obstructive pulmonary disease, Saskatchewan Canada cardiovascular disease in COPD patients. Ann Epidemiol. 2006. 16:63–70.15. Wells KB, Rogers W, Burnam MA, Camp P. Course of depression in patients with hypertension, myocardial infarction, or insulin-dependent diabetes. Am J Psychiatry. 1993. 150:632–638.16. Yohannes AM, Baldwin RC, Connolly MJ. Depression and anxiety in elderly outpatients with chronic obstructive pulmonary disease: prevalence, and validation of the BASDEC screening questionnaire. Int J Geriatr Psychiatry. 2000. 15:1090–1096.17. Al-shair K, Kolsum U, Dockry R, Morris J, Singh D, Vestbo J. Biomarkers of systemic inflammation and depression and fatigue in moderate clinically stable COPD. Respir Res. 2011. 12:3.18. Mukae H, Vincent R, Quinlan K, English D, Hards J, Hogg JC, Van Eeden SF. The effect of repeated exposure to particulate air pollution (PM10) on the bone marrow. Am J Respir Crit Care Med. 2001. 163:201–209.19. Pinto-Plata VM, Mullerova H, Toso JF, Feudjo-Tepie M, Soriano JB, Vessey RS, Celli BR. C-reactive protein in patients with COPD, control smokers and non-smokers. Thorax. 2006. 61:23–28.20. Willcox PA, Ferguson AD. Chronic obstructive airways disease following treated pulmonary tuberculosis. Respir Med. 1989. 83:195–198.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reflux esophagitis is one of highly prevalent comorbidities among patients with chronic obstructive pulmonary disease
- Chronic obstructive pulmonary disease in the older patient
- Cor Pulmonale with Particular Reference to Chronic Obstructive Pulmonary Disease and Pulmonary Tuberculosis
- A Sleepy Man with Chronic Obstructive Pulmonary Disease-Obstructive Sleep Apnea Overlap Syndrome
- Chronic Obstructive Pulmonary Disease: Respiratory Review of 2014