J Korean Med Sci.
2010 May;25(5):785-789. 10.3346/jkms.2010.25.5.785.
Malignant Rhabdoid Tumor of the Kidney Combined with Multicystic Dysplasia in a 5-year-old Child
- Affiliations
-
- 1Department of Pathology, Yonsei University Wonju College of Medicine, Wonju, Korea. soonheej@yonsei.ac.kr
- 2Department of Urology, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 3Department of Pathology, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1713967
- DOI: http://doi.org/10.3346/jkms.2010.25.5.785
Abstract
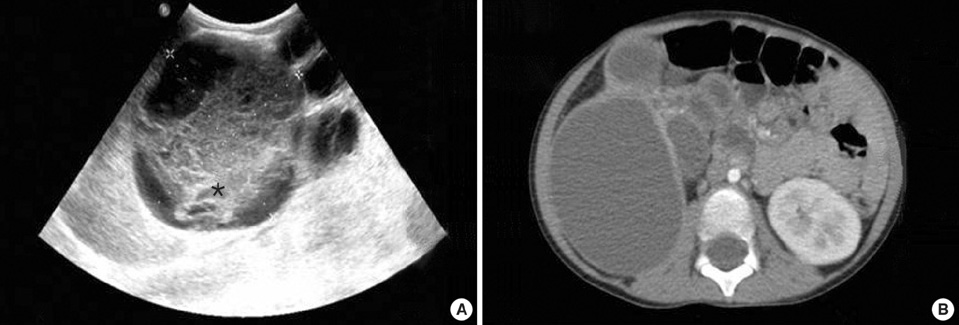
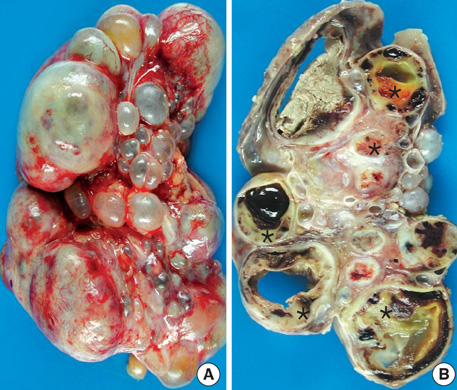
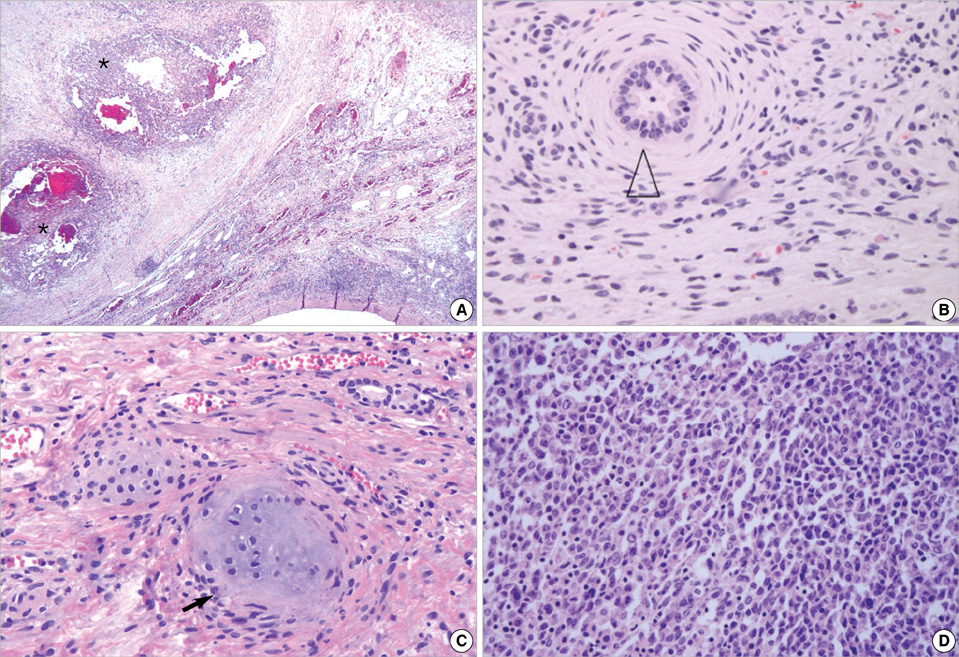
- Multicystic dysplastic kidney (MCDK) is a relatively common developmental anomaly in infants and children and has a good prognosis. In contrast, a malignant rhabdoid tumor of the kidney (MRTK) is one of the most lethal neoplasms of early life. However, the presentation of such a lethal tumor combined with multicystic dysplasia has not been reported to date. In this report, we describe a case of MRTK in a 5-yr-old girl who also had multicystic dysplasia. She was previously diagnosed with MCDK at birth due to a huge palpable mass on the right side of the abdomen. The right kidney was extensively replaced by numerous grossly dilated, variable-sized cysts. Microscopically, the tumor cells show a diffusely infiltrative growth pattern, which revealed large non-cohesive, round-to-polygonal tumor cells with vesicular nuclei. Some tumor cells had eccentric nuclei and large, round, eosinophilic cytoplasmic inclusions. There were metanephrons present, with the central ureteric bud and peripheral branches surrounded by condensing mesenchyma, immature glomeruli, and metaplastic cartilage in the adjacent parenchyma. To our knowledge, this is the first combined case of the two aforementioned diseases and this case may, in fact, suggest a new disease entity.
MeSH Terms
Figure
Reference
-
1. Welch TR, Wacksman J. The changing approach to multicystic dysplastic kidney in children. J Pediatr. 2005. 146:723–725.
Article2. Weeks DA, Beckwith JB, Mierau GW, Luckey DW. Rhabdoid tumor of kidney. A report of 111 cases from the national wilms' tumor study pathology center. Am J Surg Pathol. 1989. 13:439–458.3. Han TI, Kim MJ, Yoon HK, Chung JY, Choeh K. Rhabdoid tumour of the kidney: imaging findings. Pediatr Radiol. 2001. 31:233–237.
Article4. Narchi H. Risk of Wilms' tumour with multicystic kidney disease: a systematic review . Arch Dis Child. 2005. 90:147–149.
Article5. Robson WL, Leung AK, Thomason MA. Multicystic dysplasia of the kidney. Clin Pediatr (Phila). 1995. 34:32–40.
Article6. Gordon AC, Thomas DF, Arthur RJ, Irving HC. Multicystic dysplastic kidney: is nephrectomy still appropriate? J Urol. 1988. 140:1231–1234.
Article7. Beckwith JB. Wilms' tumor and other renal tumors of childhood: a selective review from the National Wilms' Tumor Study Pathology Center. Hum Pathol. 1983. 14:481–492.
Article8. Woolf AS, Winyard PJ. Gene expression and cell turnover in human renal dysplasia. Histol Histopathol. 2000. 15:159–166.9. Winyard PJ, Risdon RA, Sams VR, Dressler GR, Woolf AS. The PAX2 tanscription factor is expressed in cystic and hyperproliferative dysplastic epithelia in human kidney malformations. J Clin Invest. 1996. 98:451–459.
Article10. Nagata T, Takahashi Y, Ishii Y, Asai S, Sugahara-Kobayashi M, Nishida Y, Murata A, Yamamori S, Ogawa Y, Nakamura T, Murakami H, Nakamura M, Shichino H, Chin M, Sugito K, Ikeda T, Koshinaga T, Mugishima H. Molecular genetic alterations and gene expression profile of a malignant rhabdoid tumor of the kidney. Cancer Genet Cytogenet. 2005. 163:130–137.
Article11. Bostwick DG, Eble JN. Urologic surgical pathology. 1997. St. Louis; London: Mosby;21–23.12. Tomlinson GE, Breslow NE, Dome J, Guthrie KA, Norkool P, Li S, Thomas PR, Perlman E, Beckwith JB, D'Angio GJ, Green DM. Rhabdoid tumor of the kidney in the national Wilms' tumor study: age at diagnosis as a prognostic factor. J Clin Oncol. 2005. 23:7641–7645.
Article13. Gough DC, Postlethwaite RJ, Lewis MA, Bruce J. Multicystic renal dysplasia diagnosed in the antenatal period: a note of caution. Br J Urol. 1995. 76:244–248.
Article14. Rizzo N, Gabrielli S, Pilu G, Perolo A, Cacciari A, Domini R, Bovicelli L. Prenatal diagnosis and obstetrical management of multicystic dysplastic kidney disease. Prenat Diagn. 1987. 7:109–118.
Article