J Korean Med Sci.
2010 May;25(5):772-775. 10.3346/jkms.2010.25.5.772.
An Epidemiological Study of Hyperhidrosis Patients Visiting the Ajou University Hospital Hyperhidrosis Center in Korea
- Affiliations
-
- 1Hyperhidrosis Center, Ajou University Hospital, Suwon, Korea. dreunjung@paran.com
- KMID: 1713964
- DOI: http://doi.org/10.3346/jkms.2010.25.5.772
Abstract
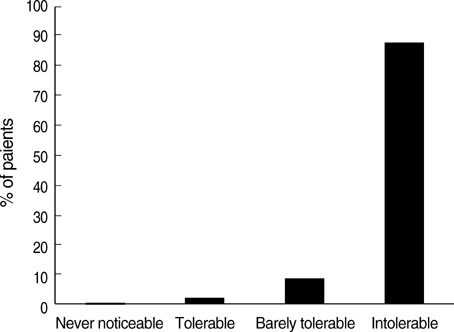
- Hyperhidrosis is a disorder of perspiration in excess of the body's physiologic need and significantly impacts one's occupational, physical, emotional, and social life. The purpose of our study was to investigate the characteristics of primary hyperhidrosis in 255 patients at Ajou University Hospital Hyperhidrosis Center from March 2006, to February 2008. Information collected from the medical records was: sex, sites of hyperhidrosis, age at visit, age of onset, aggravating factors, hyperhidrosis disease severity scale (HDSS) rank, family history, occupation, and past treatment. A total of 255 patient records were reviewed; 57.6% were male. Patients with a family history (34.1%) showed a lower age of onset (13.21+/-5.80 yr vs. 16.04+/-9.83 yr in those without family history); 16.5% had previous treatment, most commonly oriental medicine. Palmar and plantar sites were the most commonly affected, and 87.9% of patients felt their sweating was intolerable and always interfered with their daily activities. Our study provides some original information on the Korean primary hyperhidrosis population. Patients who have a family history show signs of disease in early age than those without family history.
Keyword
MeSH Terms
Figure
Reference
-
1. Haider A, Solish N. Focal hyperhidrosis: diagnosis and management. CMAJ. 2005. 172:69–75.
Article2. Strutton DR, Kowalski JW, Glaser DA, Stang PE. US prevalence of hyperhidrosis and impact on individuals with axillary hyperhidrosis: results from a national survey. J Am Acad Dermatol. 2004. 51:241–248.
Article3. Eisenach JH, Atkinson JL, Fealey RD. Hyperhidrosis: evolving therapies for a well-established phenomenon. Mayo Clin Proc. 2005. 80:657–666.
Article4. Hornberger J, Grimes K, Naumann M, Glaser DA, Lowe NJ, Naver H, Ahn S, Stolman LP. Recognition, diagnosis, and treatment of primary focal hyperhidrosis. J Am Acad Dermatol. 2004. 51:274–286.
Article5. Amir M, Arish A, Weinstein Y, Pfeffer M, Levy Y. Impairment in quality of life among patients seeking surgery for hyperhidrosis (excessive sweating): preliminary results. Isr J Psychiatry Relat Sci. 2000. 37:25–31.6. Lerer B, Jacobowitz J, Wahba A. Personality features in essential hyperhidrosis. Int J Psychiatry Med. 1980-1981. 10:59–67.
Article7. Connolly M, de Berker D. Management of primary hyperhidrosis: a summary of the different treatment modalities. Am J Clin Dermatol. 2003. 4:681–697.8. Lear W, Kessler E, Solish N, Glaser DA. An epidemiological study of hyperhidrosis. Dermatol Surg. 2007. 33:S69–S75.
Article9. Stolman LP. Treatment of hyperhidrosis. Dermatol Clin. 1998. 16:863–869.
Article10. Kaufmann H, Saadia D, Polin C, Hague S, Singleton A. Primary hyperhidrosis-evidence for autosomal dominant inheritance. Clin Auton Res. 2003. 13:96–98.11. Ro KM, Cantor RM, Lange KL, Ahn SS. Palmar hyperhidrosis: evidence of genetic transmission. J Vasc Surg. 2002. 35:382–386.
Article12. Baumgartner FJ, Bertin S, Konecny J. Superiority of thoracoscopic sympathectomy over medical management for the palmoplantar subset of severe hyperhidrosis. Ann Vasc Surg. 2009. 23:1–7.
Article13. Lee MR, Ryman WJ. Liposuction for axillary hyperhidrosis. Australas J Dermatol. 2005. 46:76–79.
Article14. Bajaj V, Langtry JA. Use of oral glycopyrronium bromide in hyperhidrosis. Br J Dermatol. 2007. 157:118–121.
Article15. Kim WO, Yoon KB, Kil HK, Yoon DM. Chemical lumbar sympathetic block in the treatment of plantar hyperhidrosis: a study of 69 patients. Dermatol Surg. 2008. 34:1340–1345.
Article16. Ellis H. Hyperhidrosis and its surgical management. Postgrad Med. 1975. 58:191–196.
Article17. Solish N, Bertucci V, Dansereau A, Hong HC, Lynde C, Lupin M, Smith KC, Storwick G. A comprehensive approach to the recognition, diagnosis, and severity-based treatment of focal hyperhidrosis: recommendations of the Canadian Hyperhidrosis Advisory Committee. Dermatol Surg. 2007. 33:908–923.
Article18. Cetindag IB, Boley TM, Webb KN, Hazelrigg SR. Long-term results and quality-of-life measures in the management of hyperhidrosis. Thorac Surg Clin. 2008. 18:217–222.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Paradoxical Responses to Oxybutynin Treatment in Localized Hyperhidrosis: Case Report
- Effect of the Third and Fourth Chain Sympathicotomy in Axillary Hyperhidrosis Accompanying Osmidrosis
- Thoracic Sympathetic Ganglion Block for a Patient with Hyperhidrosis
- A Case of Palmar Hyperhidrosis Treated with Oxybutynin in Child
- Experience of Superficial Liposuction on Compensatory Axillary Hyperhidrosis and Bromhidrosis after Thoracoscopic Sympathectomy: A case report