J Korean Med Sci.
2006 Dec;21(6):1108-1110. 10.3346/jkms.2006.21.6.1108.
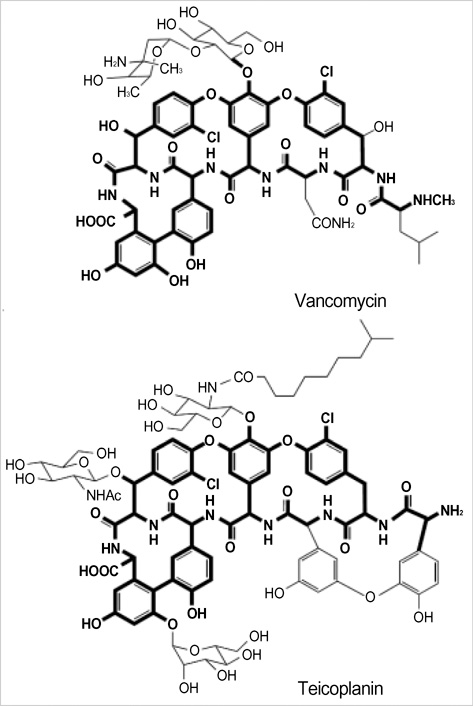
A Case of Hypersensitivity Syndrome to Both Vancomycin and Teicoplanin
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, 28 Yongun-dong Chongno-gu, Seou, Korea. drmin@snu.ac.kr
- 2Institute of Allergy and Clinical Immunology, Seoul National University Medical Research Center, Seoul, Korea.
- 3Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- 4Department of Internal Medicine, Gyeongsang National University, Jinju, Korea.
- KMID: 1713128
- DOI: http://doi.org/10.3346/jkms.2006.21.6.1108
Abstract
- Drug hypersensitivity syndrome to both vancomycin and teicoplanin has not been previously reported. We describe here a 50-yr-old male patient with vertebral osteomyelitis and epidural abscess who developed hypersensitivity syndrome to both vancomycin and teicoplanin. Skin rash, fever, eosinophilia, interstitial pneumonitis, and interstitial nephritis developed following the administration of each drug, and resolved after withdrawing the drugs and treating with high dose corticosteroids. The vertebral osteomyelitis was successfully treated with 6-week course of linezolid without further complications. Skin patch tests for vancomycin and teicoplanin was done 2 months after the recovery; a weak positive result for vancomycin (10% aq.,+at D2 and +at D4 with erythema and vesicles; ICDRG scale), and a doubtful result for teicoplanin (4% aq.-at D2 and+/-at D4 with macular erythema; ICDRG scale). We present this case to alert clinicians to the hypersensitivity syndrome that can result from vancomycin and teicoplanin, with possible cross-reactivity, which could potentially be life-threatening.
Keyword
MeSH Terms
Figure
Reference
-
1. Sullivan JR, Shear NH. The drug hypersensitivity syndrome: what is the pathogenesis? Arch Dermatol. 2001; 137:357–364.2. Hsu SI. Biopsy-proved acute tubulointerstitial nephritis and toxic epidermal necrolysis associated with vancomycin. Pharmacotherapy. 2001; 21:1233–1239.
Article3. Hannah BA, Kimmel PL, Dosa S, Turner ML. Vancomycin-induced toxic epidermal necrolysis. South Med J. 1990; 83:720–722.
Article4. Forrence EA, Goldman MP. Vancomycin-associated exfoliative dermatitis. DICP. 1990; 24:369–371.
Article5. Perrett CM, McBride SR. Teicoplanin induced drug hypersensitivity syndrome. BMJ. 2004; 328:1292.
Article6. Bachot N, Roujeau JC. Differential diagnosis of severe cutaneous drug eruptions. Am J Clin Dermatol. 2003; 4:561–572.
Article7. Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS). Semin Cutan Med Surg. 1996; 15:250–257.
Article8. McElrath MJ, Goldberg D, Neu HC. Allergic cross-reactivity of teicoplanin and vancomycin. Lancet. 1986; 1:47.
Article9. Davenport A. Allergic cross-reactivity to teicoplanin and vancomycin. Nephron. 1993; 63:482.
Article10. Marshall C, Street A, Galbraith K. Glycopeptide-induced vasculitis--cross-reactivity between vancomycin and teicoplanin. J Infect. 1998; 37:82–83.11. Khurana C, de Belder MA. Red-man syndrome after vancomycin: potential cross-reactivity with teicoplanin. Postgrad Med J. 1999; 75:41–43.
Article12. Bernedo N, Gonzalez I, Gastaminza G, Audicana M, Fernandez E, Munoz D. Positive patch test in vancomycin allergy. Contact Dermatitis. 2001; 45:43.
Article13. Hwu JJ, Chen KH, Hsu WM, Lai JY, Li YS. Ocular hypersensitivitiy to topical vancomycin in a case of chronic endophthalmitis. Cornea. 2005; 24:754–756.
Article14. Rayner CR, Baddour LM, Birmingham MC, Norden C, Meagher AK, Schentag JJ. Linezolid in the treatment of osteomyelitis: results of compassionate use experience. Infection. 2004; 32:8–14.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidence of teicoplanin adverse drug reactions among patients with vancomycin-associated adverse drug reactions and its risk factors
- Successful desensitization for vancomycin hypersensitivity
- Vancomycin-induced Hypersensitivity Reaction with Slow Infusion : A case report
- A case of vancomycin-induced drug hypersensitivity syndrome
- Teicoplanin-induced Elevation of Plasma Creatine Phosphokinase in the Patient with Wound Infection: A case report