Korean J Radiol.
2014 Feb;15(1):95-107. 10.3348/kjr.2014.15.1.95.
Terminology and Reporting Criteria for Radiofrequency Ablation of Tumors in the Scientific Literature: Systematic Review of Compliance with Reporting Standards
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 135-710, Korea. rhimhc@skku.edu
- KMID: 1711483
- DOI: http://doi.org/10.3348/kjr.2014.15.1.95
Abstract
OBJECTIVE
To perform a systematic review of compliance with standardized terminology and reporting criteria for radiofrequency (RF) tumor ablation, proposed by the International Working Group on Image-Guided Tumor Ablation in 2003, in the published reports.
MATERIALS AND METHODS
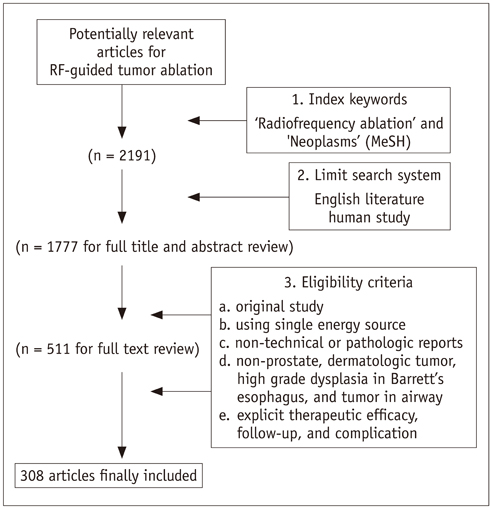
Literature search in the PubMed database was performed using index keywords, PubMed limit system, and eligibility criteria. The entire content of each article was reviewed to assess the terminology used for procedure terms, imaging findings, therapeutic efficacy, follow-up, and complications. Accuracy of the terminology and the use of alternative terms instead of standard terminology were analyzed. In addition, disparities in accuracy of terminology in articles according to the medical specialty and the type of radiology journal were evaluated.
RESULTS
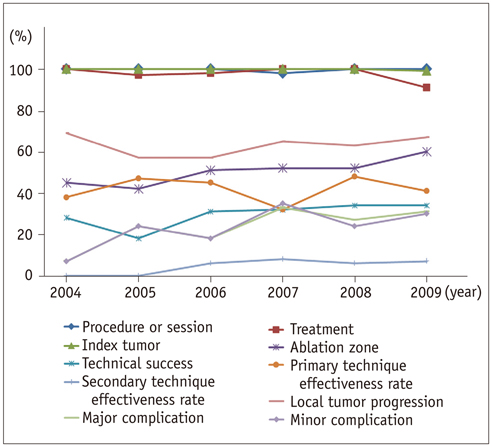
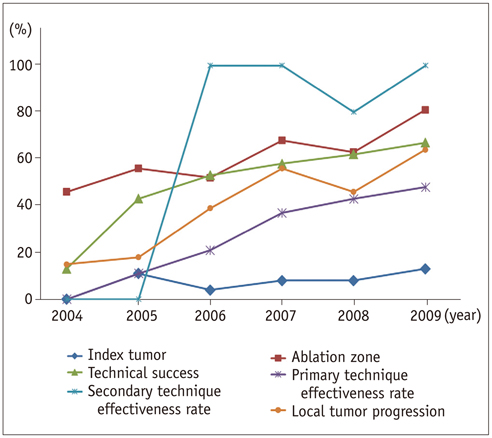
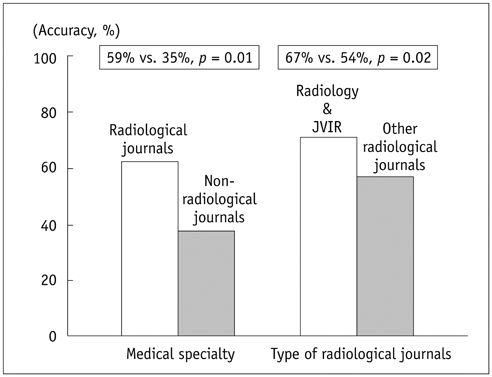
Among the articles (n = 308) included in this study, the accuracy of the terms 'procedure or session', 'treatment', 'index tumor', 'ablation zone', 'technical success', 'primary technique effectiveness rate', 'secondary technique effectiveness rate', 'local tumor progression', 'major complication', and 'minor complication' was 97% (298/307), 97% (291/300), 8% (25/307), 65% (103/159), 55% (52/94), 33% (42/129), 94% (17/18), 45% (88/195), 99% (79/80), and 100% (77/77), respectively. The overall accuracy of each term showed a tendency to improve over the years. The most commonly used alternative terms for 'technical success' and 'local tumor progression' were 'complete ablation' and 'local (tumor) recurrence', respectively. The accuracy of terminology in articles published in radiology journals was significantly greater than that of terminology in articles published in non-radiology journals, especially in Radiology and The Journal of Vascular and Interventional Radiology.
CONCLUSION
The proposal for standardization of terminology and reporting criteria for RF tumor ablation has been gaining support according to the recently published scientific reports, especially in the field of radiology. However, more work is still needed for the complete standardization of terminology.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Tumor Recurrence in Hepatocellular Carcinoma Patients after Radiofrequency Ablation: Portal Hypertension as an Indicator of Recurrence of Hepatocellular Carcinoma
Seong Won Jang, Yun Ku Cho, Ju Won Kim, Je Ryung Gil, Mi Young Kim, Young Lee
J Korean Soc Radiol. 2018;79(5):264-270. doi: 10.3348/jksr.2018.79.5.264.
Reference
-
1. Winter TC, Laeseke PF, Lee FT Jr. Focal tumor ablation: a new era in cancer therapy. Ultrasound Q. 2006; 22:195–217.2. Smith KA, Kim HS. Interventional radiology and image-guided medicine: interventional oncology. Semin Oncol. 2011; 38:151–162.3. Gillams AR. Image guided tumour ablation. Cancer Imaging. 2005; 5:103–109.4. Kurup AN, Callstrom MR. Ablation of skeletal metastases: current status. J Vasc Interv Radiol. 2010; 21:8 Suppl. S242–S250.5. Pua BB, Thornton RH, Solomon SB. Ablation of pulmonary malignancy: current status. J Vasc Interv Radiol. 2010; 21:8 Suppl. S223–S232.6. Wood BJ, Abraham J, Hvizda JL, Alexander HR, Fojo T. Radiofrequency ablation of adrenal tumors and adrenocortical carcinoma metastases. Cancer. 2003; 97:554–560.7. Lencioni R. Loco-regional treatment of hepatocellular carcinoma. Hepatology. 2010; 52:762–773.8. Schmitz AC, Gianfelice D, Daniel BL, Mali WP, van den Bosch MA. Image-guided focused ultrasound ablation of breast cancer: current status, challenges, and future directions. Eur Radiol. 2008; 18:1431–1441.9. Shen SH, Fennessy F, McDannold N, Jolesz F, Tempany C. Image-guided thermal therapy of uterine fibroids. Semin Ultrasound CT MR. 2009; 30:91–104.10. Breen DJ, Railton NJ. Minimally invasive treatment of small renal tumors: trends in renal cancer diagnosis and management. Cardiovasc Intervent Radiol. 2010; 33:896–908.11. Goldberg SN, Charboneau JW, Dodd GD 3rd, Dupuy DE, Gervais DA, Gillams AR, et al. Image-guided tumor ablation: proposal for standardization of terms and reporting criteria. Radiology. 2003; 228:335–345.12. Goldberg SN, Grassi CJ, Cardella JF, Charboneau JW, Dodd GD 3rd, Dupuy DE, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria. J Vasc Interv Radiol. 2005; 16:765–778.13. Goldberg SN, Grassi CJ, Cardella JF, Charboneau JW, Dodd GD 3rd, Dupuy DE, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria. Radiology. 2005; 235:728–739.14. Goldberg SN, Grassi CJ, Cardella JF, Charboneau JW, Dodd GD 3rd, Dupuy DE, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria. J Vasc Interv Radiol. 2009; 20:7 Suppl. S377–S390.15. Strasberg SM, Phillips C. Use and dissemination of the brisbane 2000 nomenclature of liver anatomy and resections. Ann Surg. 2013; 257:377–382.16. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009; 151:264–269.17. Halligan S, Altman DG. Evidence-based practice in radiology: steps 3 and 4--appraise and apply systematic reviews and meta-analyses. Radiology. 2007; 243:13–27.18. Staunton M. Evidence-based radiology: steps 1 and 2--asking answerable questions and searching for evidence. Radiology. 2007; 242:23–31.19. Blana A, Brown SC, Chaussy C, Conti GN, Eastham JA, Ganzer R, et al. High-intensity focused ultrasound for prostate cancer: comparative definitions of biochemical failure. BJU Int. 2009; 104:1058–1062.20. Mathur PN, Edell E, Sutedja T, Vergnon JM. American College of Chest Physicians. Treatment of early stage non-small cell lung cancer. Chest. 2003; 123:1 Suppl. 176S–180S.21. Shaheen NJ, Sharma P, Overholt BF, Wolfsen HC, Sampliner RE, Wang KK, et al. Radiofrequency ablation in Barrett's esophagus with dysplasia. N Engl J Med. 2009; 360:2277–2288.22. World Health Organization. WHO Handbook for Reporting Results of Cancer Treatment, WHO Offset publication No 48. Geneva: WHO;1979.23. Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. European Organization for Research and Treatment of Cancer. National Cancer Institute of the United States. National Cancer Institute of Canada. New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst. 2000; 92:205–216.24. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009; 45:228–247.25. Burke DR, Lewis CA, Cardella JF, Citron SJ, Drooz AT, Haskal ZJ, et al. Quality improvement guidelines for percutaneous transhepatic cholangiography and biliary drainage. Society of Cardiovascular and Interventional Radiology. J Vasc Interv Radiol. 1997; 8:677–681.26. Leoni CJ, Potter JE, Rosen MP, Brophy DP, Lang EV. Classifying complications of interventional procedures: a survey of practicing radiologists. J Vasc Interv Radiol. 2001; 12:55–59.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Literature Analysis on Reporting Standards for Qualitative Research in Cancer-related Studies
- Meta-epidemiology
- Reporting Quality of Diagnostic Accuracy Studies in Laboratory Medicine: Adherence to Standards for Reporting of Diagnostic Accuracy Studies (STARD) 2015
- Reporting Guidelines for Survey Reporting (G-SURE): protocol for guideline development
- Radiofrequency in arthroscopic shoulder surgery: a systematic review