Korean J Radiol.
2014 Feb;15(1):37-44. 10.3348/kjr.2014.15.1.37.
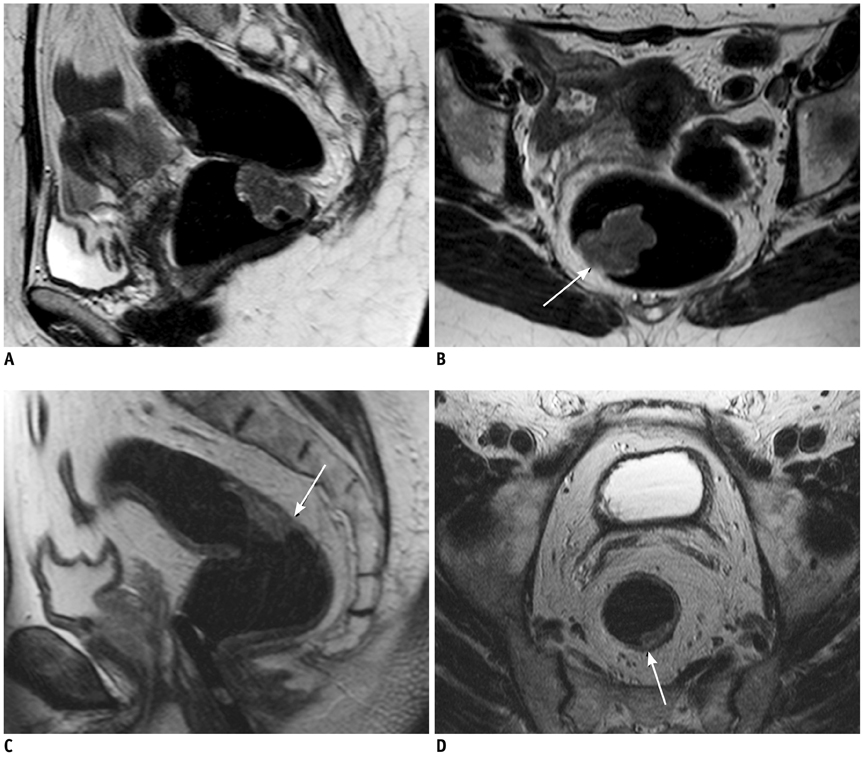
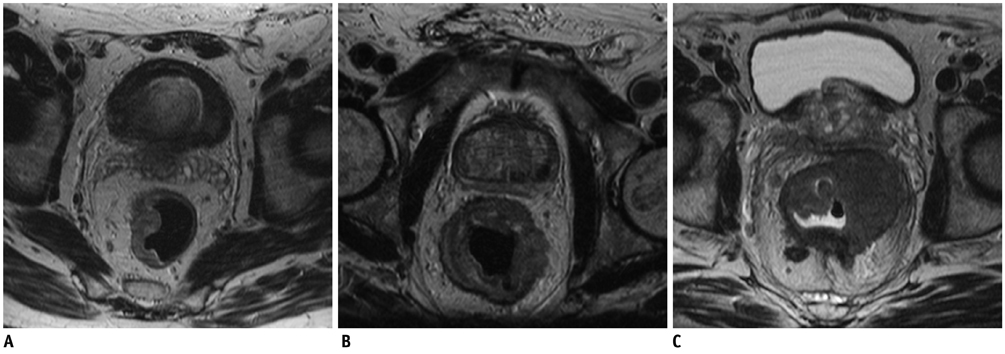
Accuracy of High-Resolution MRI with Lumen Distention in Rectal Cancer Staging and Circumferential Margin Involvement Prediction
- Affiliations
-
- 1Radiology Institute, Faculty of Medicine and Psychology, University of Rome, Sapienza, Sant'Andrea Hospital, Rome 00189, Italy. elsa.iannicelli@uniroma1.it
- 2Department of Surgical and Medical Sciences and Translational Medicine, Faculty of Medicine and Psychology, University of Rome, Sapienza, Sant'Andrea Hospital, Rome 00189, Italy.
- 3Department of Clinical and Molecular Sciences, Faculty of Medicine and Psychology, University of Rome, Sapienza, Sant'Andrea Hospital, Rome 00189, Italy.
- KMID: 1711475
- DOI: http://doi.org/10.3348/kjr.2014.15.1.37
Abstract
OBJECTIVE
To evaluate the accuracy of magnetic resonance imaging (MRI) with lumen distention for rectal cancer staging and circumferential resection margin (CRM) involvement prediction.
MATERIALS AND METHODS
Seventy-three patients with primary rectal cancer underwent high-resolution MRI with a phased-array coil performed using 60-80 mL room air rectal distention, 1-3 weeks before surgery. MRI results were compared to postoperative histopathological findings. The overall MRI T staging accuracy was calculated. CRM involvement prediction and the N staging, the accuracy, sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were assessed for each T stage. The agreement between MRI and histological results was assessed using weighted-kappa statistics.
RESULTS
The overall MRI accuracy for T staging was 93.6% (k = 0.85). The accuracy, sensitivity, specificity, PPV and NPV for each T stage were as follows: 91.8%, 86.2%, 95.5%, 92.6% and 91.3% for the group < or = T2; 90.4%, 94.6%, 86.1%, 87.5% and 94% for T3; 98,6%, 85.7%, 100%, 100% and 98.5% for T4, respectively. The predictive CRM accuracy was 94.5% (k = 0.86); the sensitivity, specificity, PPV and NPV were 89.5%, 96.3%, 89.5%, and 96.3% respectively. The N staging accuracy was 68.49% (k = 0.4).
CONCLUSION
MRI performed with rectal lumen distention has proved to be an effective technique both for rectal cancer staging and involved CRM predicting.
Keyword
MeSH Terms
Figure
Reference
-
1. Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010; 60:277–300.2. Quirke P, Durdey P, Dixon MF, Williams NS. Local recurrence of rectal adenocarcinoma due to inadequate surgical resection. Histopathological study of lateral tumour spread and surgical excision. Lancet. 1986; 2:996–999.3. Kong M, Hong SE, Choi WS, Kim SY, Choi J. Preoperative concurrent chemoradiotherapy for locally advanced rectal cancer: treatment outcomes and analysis of prognostic factors. Cancer Res Treat. 2012; 44:104–112.4. Church JM, Gibbs P, Chao MW, Tjandra JJ. Optimizing the outcome for patients with rectal cancer. Dis Colon Rectum. 2003; 46:389–402.5. Muthusamy VR, Chang KJ. Optimal methods for staging rectal cancer. Clin Cancer Res. 2007; 13(22 Pt 2):6877s–6884s.6. Nagtegaal ID, Marijnen CA, Kranenbarg EK, van de Velde CJ, van Krieken JH, et al. Pathology Review Committee. Circumferential margin involvement is still an important predictor of local recurrence in rectal carcinoma: not one millimeter but two millimeters is the limit. Am J Surg Pathol. 2002; 26:350–357.7. Nagtegaal ID, Quirke P. What is the role for the circumferential margin in the modern treatment of rectal cancer? J Clin Oncol. 2008; 26:303–312.8. Slater A, Halligan S, Taylor SA, Marshall M. Distance between the rectal wall and mesorectal fascia measured by MRI: Effect of rectal distension and implications for preoperative prediction of a tumour-free circumferential resection margin. Clin Radiol. 2006; 61:65–70.9. Beets-Tan RG, Beets GL, Vliegen RF, Kessels AG, Van Boven H, De Bruine A, et al. Accuracy of magnetic resonance imaging in prediction of tumour-free resection margin in rectal cancer surgery. Lancet. 2001; 357:497–504.10. Brown G, Radcliffe AG, Newcombe RG, Dallimore NS, Bourne MW, Williams GT. Preoperative assessment of prognostic factors in rectal cancer using high-resolution magnetic resonance imaging. Br J Surg. 2003; 90:355–364.11. Rao SX, Zeng MS, Xu JM, Qin XY, Chen CZ, Li RC, et al. Assessment of T staging and mesorectal fascia status using high-resolution MRI in rectal cancer with rectal distention. World J Gastroenterol. 2007; 13:4141–4146.12. Kim MJ, Lim JS, Oh YT, Kim JH, Chung JJ, Joo SH, et al. Preoperative MRI of rectal cancer with and without rectal water filling: an intraindividual comparison. AJR Am J Roentgenol. 2004; 182:1469–1476.13. Wallengren NO, Holtås S, Andrén-Sandberg A, Jonsson E, Kristoffersson DT, McGill S. Rectal carcinoma: double-contrast MR imaging for preoperative staging. Radiology. 2000; 215:108–114.14. Goh JS, Goh JP, Wansaicheong GK. Methylcellulose as a rectal contrast agent for MR imaging of rectal carcinoma. AJR Am J Roentgenol. 2002; 178:1145–1146.15. Kaur H, Choi H, You YN, Rauch GM, Jensen CT, Hou P, et al. MR imaging for preoperative evaluation of primary rectal cancer: practical considerations. Radiographics. 2012; 32:389–409.16. American Joint Committee on Cancer. Colon and Rectum. AJCC cancer staging Handbook. 6th ed. New York: Springer-Verlag;2002. p. 127–138.17. American Joint Committee on Cancer. Colon and Rectum. AJCC cancer staging manual. 7th ed. New York, NY: Springer;2010. p. 143–164.18. Quirke P, Morris E. Reporting colorectal cancer. Histopathology. 2007; 50:103–112.19. Ferri M, Laghi A, Mingazzini P, Iafrate F, Meli L, Ricci F, et al. Pre-operative assessment of extramural invasion and sphincteral involvement in rectal cancer by magnetic resonance imaging with phased-array coil. Colorectal Dis. 2005; 7:387–393.20. Akasu T, Iinuma G, Takawa M, Yamamoto S, Muramatsu Y, Moriyama N. Accuracy of high-resolution magnetic resonance imaging in preoperative staging of rectal cancer. Ann Surg Oncol. 2009; 16:2787–2794.21. Klessen C, Rogalla P, Taupitz M. Local staging of rectal cancer: the current role of MRI. Eur Radiol. 2007; 17:379–389.22. MERCURY Study Group. Extramural depth of tumor invasion at thin-section MR in patients with rectal cancer: results of the MERCURY study. Radiology. 2007; 243:132–139.23. Adam IJ, Mohamdee MO, Martin IG, Scott N, Finan PJ, Johnston D, et al. Role of circumferential margin involvement in the local recurrence of rectal cancer. Lancet. 1994; 344:707–711.24. Oh YT, Kim MJ, Lim JS, Kim JH, Lee KY, Kim NK, et al. Assessment of the prognostic factors for a local recurrence of rectal cancer: the utility of preoperative MR imaging. Korean J Radiol. 2005; 6:8–16.25. Brown G. Thin section MRI in multidisciplinary pre-operative decision making for patients with rectal cancer. Br J Radiol. 2005; 78(Spec No 2):S117–S127.26. Suzuki C, Torkzad MR, Tanaka S, Palmer G, Lindholm J, Holm T, et al. The importance of rectal cancer MRI protocols on interpretation accuracy. World J Surg Oncol. 2008; 6:89.27. Vliegen RF, Beets GL, von Meyenfeldt MF, Kessels AG, Lemaire EE, van Engelshoven JM, et al. Rectal cancer: MR imaging in local staging--is gadolinium-based contrast material helpful? Radiology. 2005; 234:179–188.28. Bellows CF, Jaffe B, Bacigalupo L, Pucciarelli S, Gagliardi G. Clinical significance of magnetic resonance imaging findings in rectal cancer. World J Radiol. 2011; 3:92–104.29. Harewood GC, Kumar KS, Clain JE, Levy MJ, Nelson H. Clinical implications of quantification of mesorectal tumor invasion by endoscopic ultrasound: all T3 rectal cancers are not equal. J Gastroenterol Hepatol. 2004; 19:750–755.30. Beets-Tan RG. MRI in rectal cancer: the T stage and circumferential resection margin. Colorectal Dis. 2003; 5:392–395.31. Fernández-Esparrach G, Ayuso-Colella JR, Sendino O, Pagés M, Cuatrecasas M, Pellisé M, et al. EUS and magnetic resonance imaging in the staging of rectal cancer: a prospective and comparative study. Gastrointest Endosc. 2011; 74:347–354.32. Shihab OC, Moran BJ, Heald RJ, Quirke P, Brown G. MRI staging of low rectal cancer. Eur Radiol. 2009; 19:643–650.33. Al-Sukhni E, Milot L, Fruitman M, Beyene J, Victor JC, Schmocker S, et al. Diagnostic accuracy of MRI for assessment of T category, lymph node metastases, and circumferential resection margin involvement in patients with rectal cancer: a systematic review and meta-analysis. Ann Surg Oncol. 2012; 19:2212–2223.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Significance of Preoperative Magnetic Resonance Imaging in Staging of Rectal Cancer
- Diagnostic Performance of Rectal CT for Staging Rectal Cancer: Comparison with Rectal MRI and Histopathology
- Preoperative Evaluation of Lower Rectal Cancer by Pelvic MR with and without Gel Filling
- Diagnostic Accuracy of Computed Tomography and Magnetic Resonance Imaging Obtained after Neoadjuvant Chemoradiotherapy in Predicting the Local Tumor Stage and Circumferential Resection Margin Status of Rectal Cancer
- Preoperative Staging of Rectal Cancer by CT & MRI