J Korean Soc Radiol.
2014 Jul;71(1):20-25. 10.3348/jksr.2014.71.1.20.
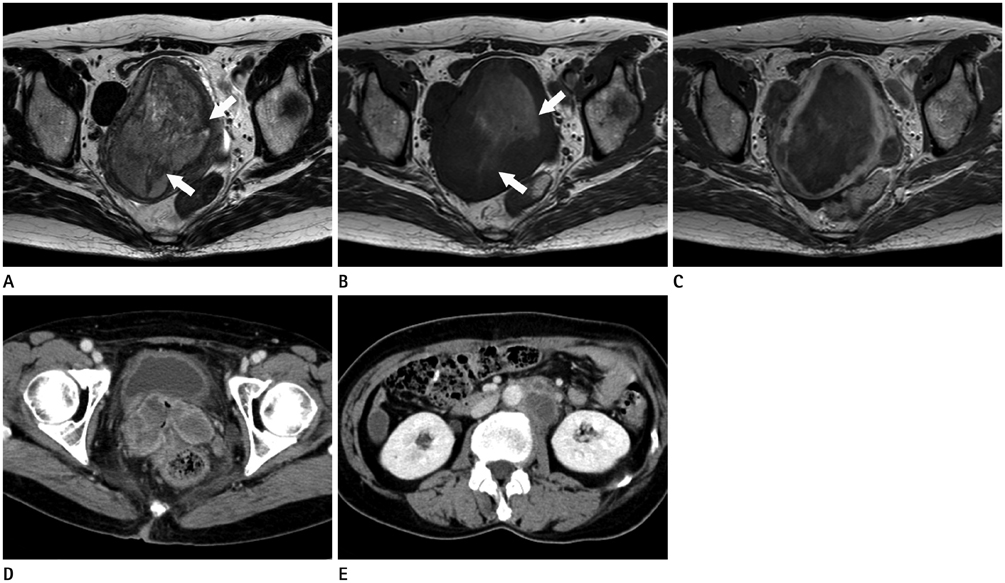
Malignant Extrarenal Rhabdoid Tumor in Adults: Three Case Reports Originating from the Ileum, Adrenal Gland and Uterus
- Affiliations
-
- 1Department of Radiology, Ansan Hospital, Korea University College of Medicine, Ansan, Korea. pagoda20@gmail.com
- 2Department of Colorectal Surgery, Ansan Hospital, Korea University College of Medicine, Ansan, Korea.
- 3Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 4Department of Pathology, Ansan Hospital, Korea University College of Medicine, Ansan, Korea.
- KMID: 1709016
- DOI: http://doi.org/10.3348/jksr.2014.71.1.20
Abstract
- Malignant extrarenal rhabdoid tumor (MERT) is a very aggressive tumor that is extremely rare in adults. Herein, we introduce three cases of MERT in adults that originated in the ileum, adrenal gland, and uterine endometrium. The MERTs in the ileum and adrenal gland showed non-aggressive features and a good prognosis, while the MERT in the uterine presented with aggressive features and distant metastasis.
MeSH Terms
Figure
Reference
-
1. Abdullah A, Patel Y, Lewis TJ, Elsamaloty H, Strobel S. Extrarenal malignant rhabdoid tumors: radiologic findings with histopathologic correlation. Cancer Imaging. 2010; 10:97–101.2. Haas JE, Palmer NF, Weinberg AG, Beckwith JB. Ultrastructure of malignant rhabdoid tumor of the kidney. A distinctive renal tumor of children. Hum Pathol. 1981; 12:646–657.3. Biegel JA, Kalpana G, Knudsen ES, Packer RJ, Roberts CW, Thiele CJ, et al. The role of INI1 and the SWI/SNF complex in the development of rhabdoid tumors: meeting summary from the workshop on childhood atypical teratoid/rhabdoid tumors. Cancer Res. 2002; 62:323–328.4. Gadd S, Sredni ST, Huang CC, Perlman EJ. Renal Tumor Committee of the Children's Oncology Group. Rhabdoid tumor: gene expression clues to pathogenesis and potential therapeutic targets. Lab Invest. 2010; 90:724–738.5. Ogino S, Ro TY, Redline RW. Malignant rhabdoid tumor: A phenotype? An entity?--A controversy revisited. Adv Anat Pathol. 2000; 7:181–190.6. Fanburg-Smith JC, Hengge M, Hengge UR, Smith JS Jr, Miettinen M. Extrarenal rhabdoid tumors of soft tissue: a clinicopathologic and immunohistochemical study of 18 cases. Ann Diagn Pathol. 1998; 2:351–362.7. Tóth L, Nemes Z, Gomba S, Asztalos L, Molnár C, András C, et al. Primary rhabdoid cancer of the ileum: a case report and review of the literature. Pathol Res Pract. 2010; 206:110–115.8. Salamanca J, Nevado M, Martínez-González MA, Pérez-Espejo G, Pinedo F. Undifferentiated carcinoma of the jejunum with extensive rhabdoid features. Case report and review of the literature. APMIS. 2008; 116:941–946.9. Yaris N, Cobanoglu U, Dilber E, Ahmetoğlu A, Saruhan H, Okten A. Malignant rhabdoid tumor of adrenal gland. Med Pediatr Oncol. 2002; 39:128–131.10. Horazdovsky R, Manivel JC, Cheng EY. Successful salvage and long-term survival after recurrent malignant rhabdoid tumor. Sarcoma. 2007; 2007:53549.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Malignant Extrarenal Rhabdoid Tumor of the Retroperitoneum
- Imaging Findings of a Malignant Rhabdoid Tumor in the Stomach: A Case Report
- A Case of Malignant Extrarenal Rhabdoid Tumor
- A Case of Malignant Rhabdoid Tumor on the Face
- Malignant Extrarenal Rhabdoid Tumor of the Pelvic Paravertebral Region: Case Report