Korean J Ophthalmol.
2013 Oct;27(5):381-383. 10.3341/kjo.2013.27.5.381.
A Case of Susac Syndrome
- Affiliations
-
- 1Department of Ophthalmology, Kim's Eye Hospital, Konyang University College of Medicine, Seoul, Korea. ccnnrr@naver.com
- KMID: 1707294
- DOI: http://doi.org/10.3341/kjo.2013.27.5.381
Abstract
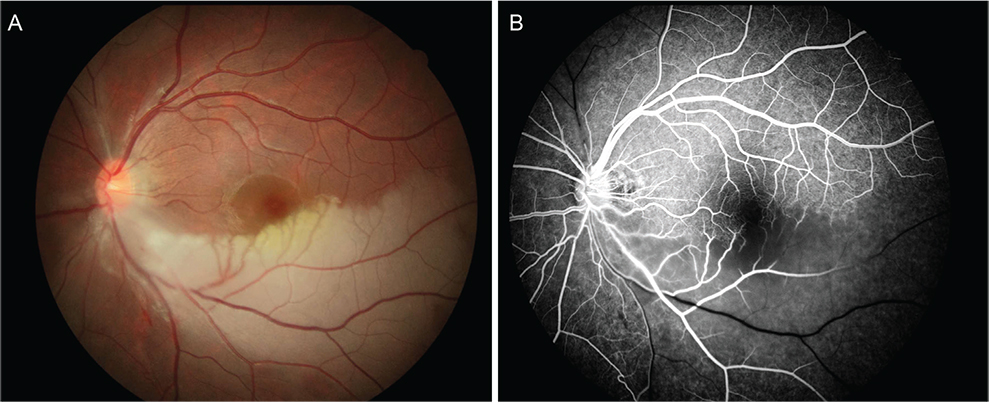
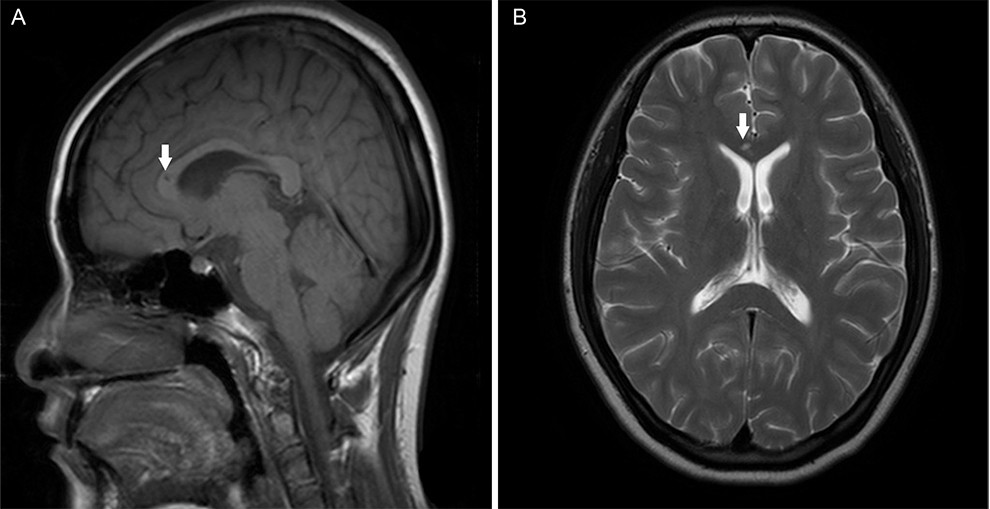
- The purpose of this article is to report on the first known Korean case of Susac syndrome. An 18-year-old female came to our clinic reporting blurred vision of the left eye for 2 days. She also complained of decreased hearing with tinnitus of the right ear and mild headache. She was previously healthy and had no remarkable medical history. Best-corrected visual acuity was 20 / 50 in the left eye and 20 / 20 in the right eye. An axiomatic triad of ocular, cochlear, and neurologic involvement was observed in the patient. Fluorescein angiography showed branched retinal arterial occlusions in the left eye. A sudden right sensorineural hearing loss was observed on audimetry. Magnetic resonance images showed a hyperintense lesion in the white matter around the corpus callosum. The patient was treated with high doses of systemic corticosteroids, and no neuropsychological sequelae were observed. This is the first case report of Susac syndrome in Korea. In cases of retinal arterial occlusion with hearing loss or neuropsychological symptoms, Susac syndrome should be suspected.
MeSH Terms
Figure
Reference
-
1. Susac JO, Hardman JM, Selhorst JB. Microangiopathy of the brain and retina. Neurology. 1979; 29:313–316.2. Murata Y, Inada K, Negi A. Susac syndrome. Am J Ophthalmol. 2000; 129:682–684.3. O'Halloran HS, Pearson PA, Lee WB, et al. Microangiopathy of the brain, retina, and cochlea (Susac syndrome): a report of five cases and a review of the literature. Ophthalmology. 1998; 105:1038–1044.4. Do TH, Fisch C, Evoy F. Susac syndrome: report of four cases and review of the literature. AJNR Am J Neuroradiol. 2004; 25:382–388.5. Papo T, Biousse V, Lehoang P, et al. Susac syndrome. Medicine (Baltimore). 1998; 77:3–11.6. Saw VP, Canty PA, Green CM, et al. Susac syndrome: microangiopathy of the retina, cochlea and brain. Clin Experiment Ophthalmol. 2000; 28:373–381.7. Susac JO, Murtagh FR, Egan RA, et al. MRI findings in Susac's syndrome. Neurology. 2003; 61:1783–1787.8. Egan RA, Ha Nguyen T, Gass JD, et al. Retinal arterial wall plaques in Susac syndrome. Am J Ophthalmol. 2003; 135:483–486.9. McLeod DS, Ying HS, McLeod CA, et al. Retinal and optic nerve head pathology in Susac's syndrome. Ophthalmology. 2011; 118:548–552.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recurrent Bilateral Branch Retinal Artery Occlusion with Hearing Loss and Encephalopathy: The First Case Report of Susac Syndrome in Korea
- Letter to the Editor: Sneddon's Syndrome versus Susac Syndrome
- Susac Syndrome With Retinal Vasculitis: A Rare Case Report and Brief Review
- Susac Syndrome With Good Response to Intravenous Immunoglobulin: A Case Report
- Neurological Adverse Reactions to SARS-CoV-2 Vaccines