Korean J Hematol.
2005 Sep;40(3):205-209. 10.5045/kjh.2005.40.3.205.
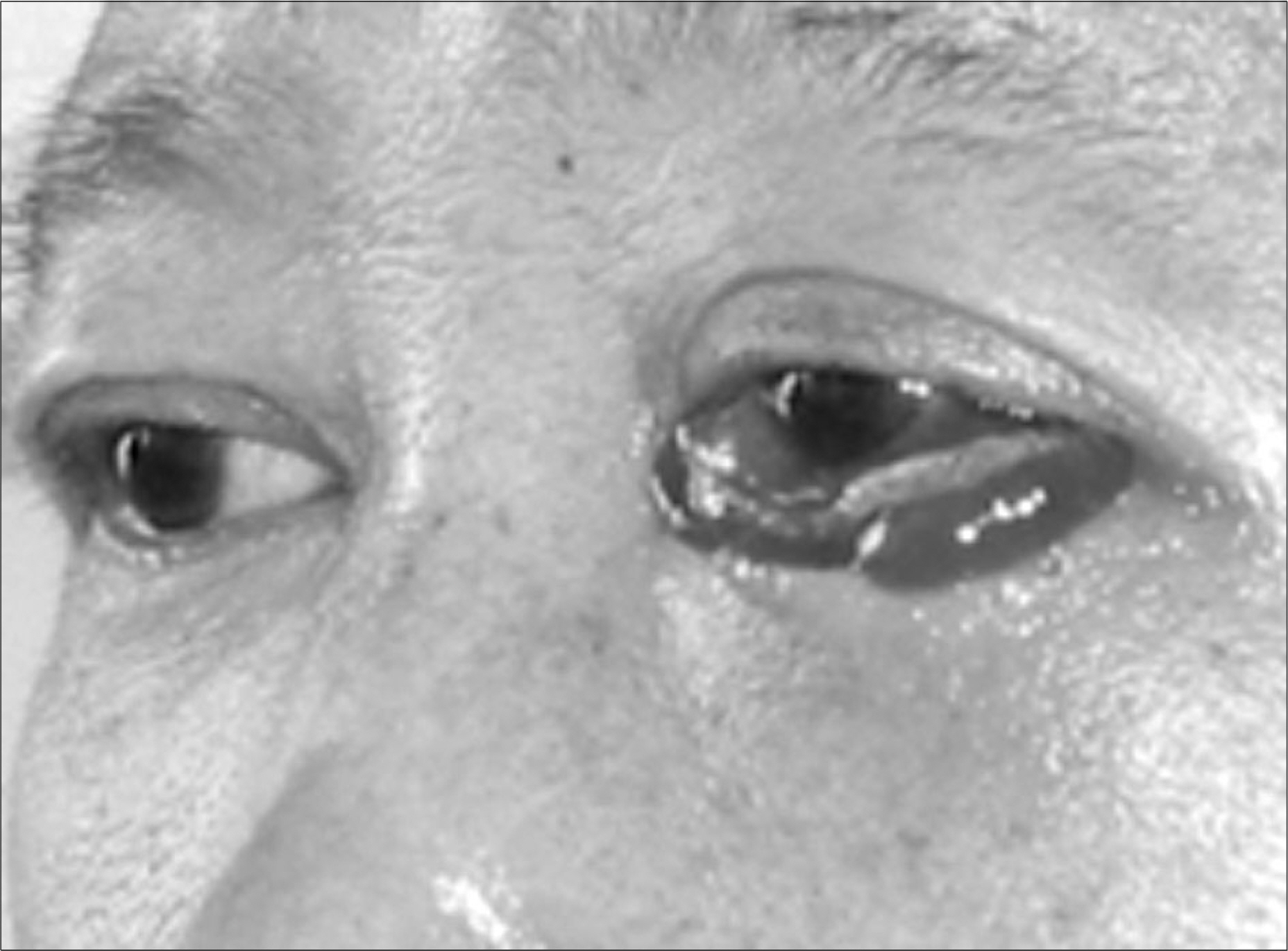
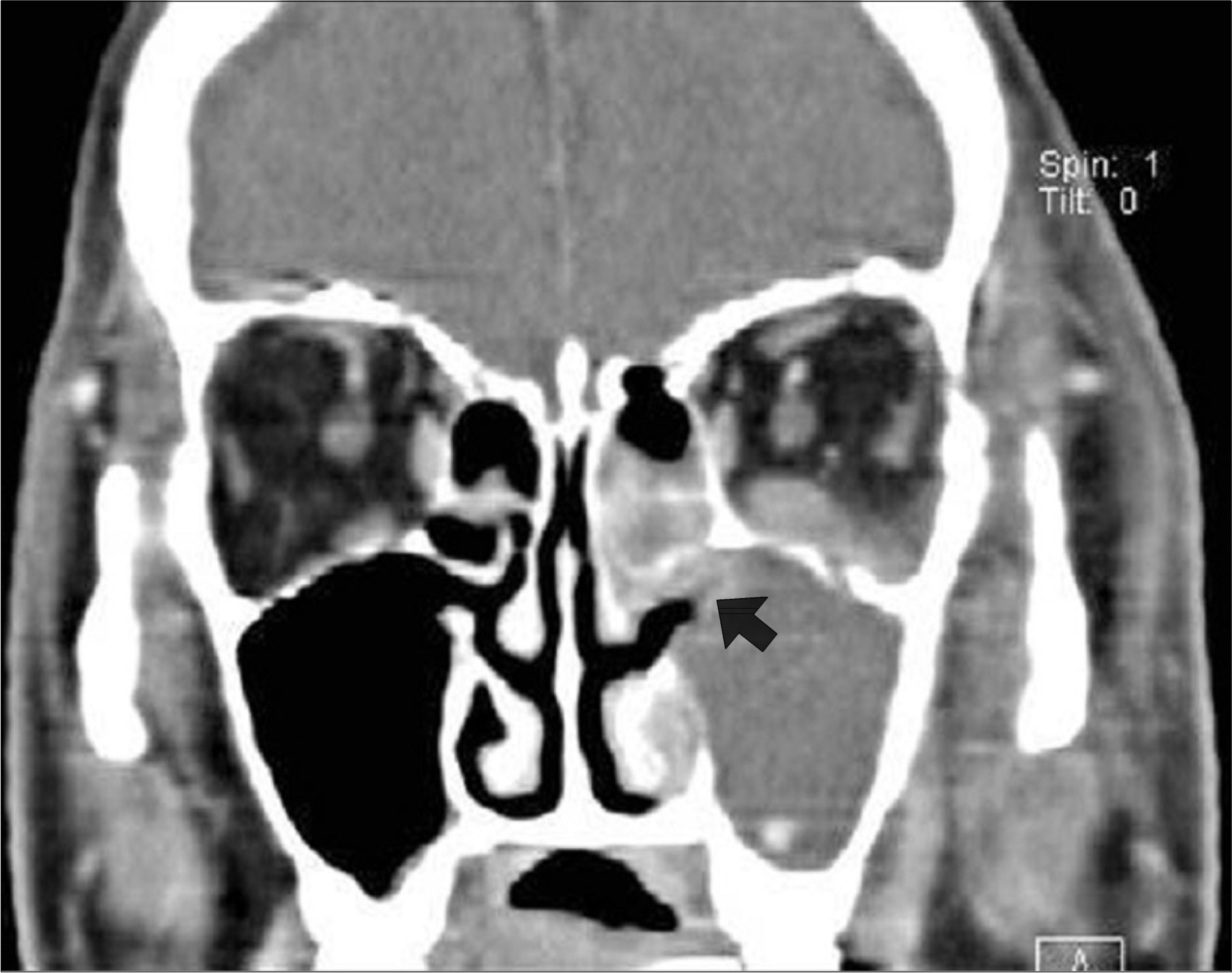
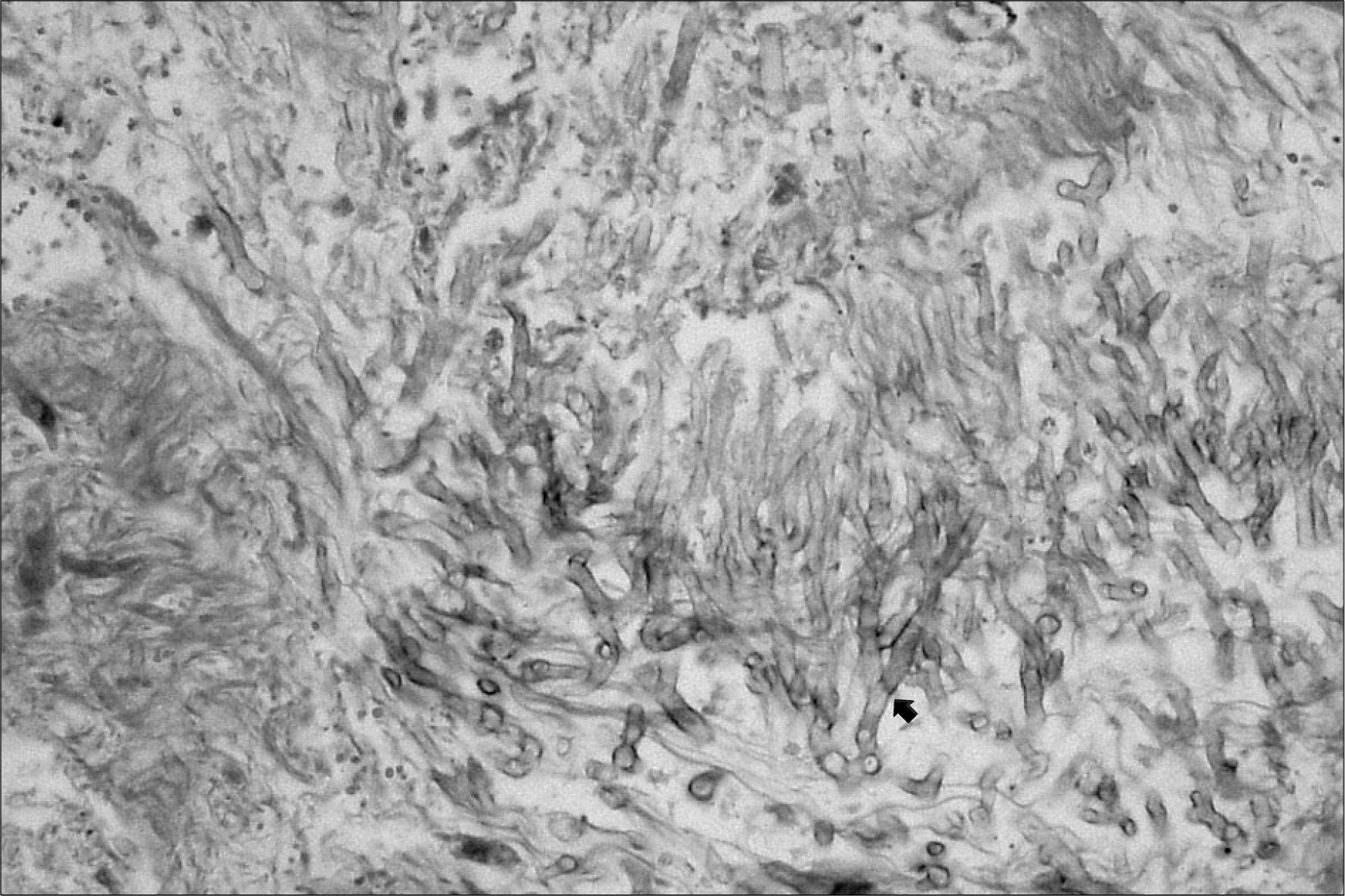
A Case of Invasive Maxillary and Orbital Aspergillosis Inhematopoietic Stem Cell Transplantation Recipient with Severe Aplastic Anemia
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, Inje University, Busan, Korea. yjoo@inje.ac.kr
- 2Department of Ophthalmology, College of Medicine, Inje University, Busan, Korea.
- 3Department of Otorhinolaryngology, College of Medicine, Inje University, Busan, Korea.
- KMID: 1610819
- DOI: http://doi.org/10.5045/kjh.2005.40.3.205
Abstract
- Invasive aspergillosis (IA) of the paranasal sinuses is a rare infectious complication associated with allogeneic hematopoietic stem cell transplantation (HSCT). However, immunocompromised patients are particularly at risk of fulminant IA. The high risk of an invasive fungal infection (IFI) following allogeneic HSCT is due to several factors, including neutropenia before engraftment, disruption of mucosal barriers by various preparative regimens and the use of broad-spectrum antimicrobial agents, as well as the immunosuppressive effects of prophylaxis and treatment of GVHD. As the therapy for an IFI following allogeneic HSCT is often unsuccessful, the mortality rate is increased by 95%. Therefore, early diagnosis is important to overcome the high mortality of this destructive disease. In previous studies, high risks for the early onset of IA were demonstrated in patients with severe aplastic anemia (SAA), independent of the day of engraftment. Here, we report a case of invasive aspergillosis of the maxillary sinuses and orbit in a 50 years old man with SAA, who underwent an allogeneic HSCT from a HLA-matched sibling conditioned with Cytoxan/Fludara/ATG.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Invasive Aspergillosis of the Paranasal Sinuses Invading Skull Base : Successful Treatment with Voriconazole
Chai Ryoung Eun, Jung Yeon Heo, Ji Yun Noh, Young Kyung Youn, Hyun Joo Lee, Bong Kyung Shin, Jacob Lee, Joon Young Song, Hee Jin Cheong, Woo Joo Kim
Infect Chemother. 2008;40(2):110-115. doi: 10.3947/ic.2008.40.2.110.
Reference
-
1). Martinez D, Burgueno M, Martin M, Sierra I. Invasive maxillary aspergillosis after dental extraction. Oral Surg Oral Med Oral Pathol. 1992; 74:466–8.
Article2). Notani K, Satoh C, Hashimoto I, et al. Intracranial aspergillus infection from the paranasal sinus. Oral Surg Oral Med Oral Pathol. 2000; 89:9–ll.
Article3). Meyer RD. A. pergillus species. Gordobach SL, Bartlett JG, Blacklow NR, editors. Infectious diseases. 2nd ed.Philadelphia, PA: Saunders;2006. p. 2327–34.4). Latge JP. Aspergillus fumigatus and aspergillosis. Clin Microbial Rev. 1999; 12:310–50.5). Sterman BM. Sinus surgery in bone marrow transplantation patients. Am J Rhinol. 1999; 13:351–7.
Article6). Talbot GH, Huang A, Provencher M. Invasive aspergillus rhinosinusitis in patients with acute leukemia. Rev Infect Dis. 1991; 13:219–32.
Article7). Napoli JA, Donegan JO. Aspergillosis and necrosis of the maxilla: a case report. J Oral Maxillofac Surg. 1991; 49:532–4.
Article8). Myoken Y, Sugata T, Kyo T, Fujihara M. Pathologic features of invasive oral aspergillosis in patients with hematologic malignancies. J Oral Maxillofac Surg. 1996; 54:263–70.
Article9). Walsh TJ, Pizzo PA. Nosocomial fungal infections: a classification for hospital-acquired fungal infections and mycoses arising from endogenous flora or reactivation. An nu Rev Microbiol. 1988; 42:517–45.
Article10). Waxman JE, Specter JG, Sale SR, Katzenstein AL. Allergic aspergillus sinusitis. Concepts in diagnosis and treatment of a new clinical entity. Laryngoscope. 1987; 97:261–6.11). Talbot GH, Huang A, Plovench M. Invasive aspergillus rhinosinusitis in patients with acute leukemia. Rev Infect Dis. 1991; 13:219–32.
Article12). Henderson VJ, Hirvela ER. Emerging and reemerging microbial threats. Nosocomial fungus infections. Arch Surg. 1996; 131:330–7.13). Marr AM, Patterson T, Denning D. Aspergillosis, pathogenesis, clinical manifestations, and therapy. Infect Dis Clin North Am. 2002; 16:875–94.14). Ellis M, Richardson M, de Pauw B. Epidemiology. Hosp Med. 2000; 61:605–9.
Article15). Dimitrakopoulos I, Lazaride N, Asimaki A. Craniofacial invasive aspergillosis in an immunocompetent patient. A case report. J. Oral Maxillofac Surg. 2005; 63:845–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Allogeneic Hematopoietic Stem Cell Transplantation for a Patient with Very Severe Aplastic Anemia During Active Invasive Fungal Infection
- Papillary Thyroid Cancer in a Child with Very Severe Aplastic Anemia
- Successful engraftment after infusion of multiple low doses of CD34+ cells from a poorly matched sibling donor in a patient with severe aplastic anemia
- Disseminated Aspergillosis following Allogeneic Hematopoietic Stem Cell Transplantation in an Acute Leukemic Patient who was Previously Treated for Invasive Aspergillosis
- A Case of Invasive Pulmonary Aspergillosis Cured with Liposomal Amphotericin, Granulocyte Transfusion and Surgery in an Allogeneic Hemopoietic Stem Cell Transplantation Recipient