Yonsei Med J.
2013 Mar;54(2):453-463. 10.3349/ymj.2013.54.2.453.
Rapid Decrease of Intact Parathyroid Hormone Could Be a Predictor of Better Response to Cinacalcet in Hemodialysis Patients
- Affiliations
-
- 1Department of Internal Medicine & Kidney Research Institute, Hallym University College of Medicine, Anyang, Korea.
- 2Department of Internal Medicine, Korea University Medical School, Seoul, Korea.
- 3Department of Internal Medicine, Chonnam National University Medical School, Gwangjuv, Korea.
- 4Department of Nephrology, College of Medicine, Busan Paik Hospital, Inje University, Busan, Korea.
- 5Division of Nephrology, Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 6Department of Internal Medicine, School of Medicine, Ewha Womans University, Seoul, Korea.
- 7Department of Internal Medicine, Soonchunhyang University Bucheon Hospital, Bucheon, Korea.
- 8Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. khchoi6@yuhs.ac
- KMID: 1503910
- DOI: http://doi.org/10.3349/ymj.2013.54.2.453
Abstract
- PURPOSE
Cinacalcet is effective for treating refractory secondary hyperparathyroidism (SHPT), but little is known about the response rates and clinical factors influencing the response.
MATERIALS AND METHODS
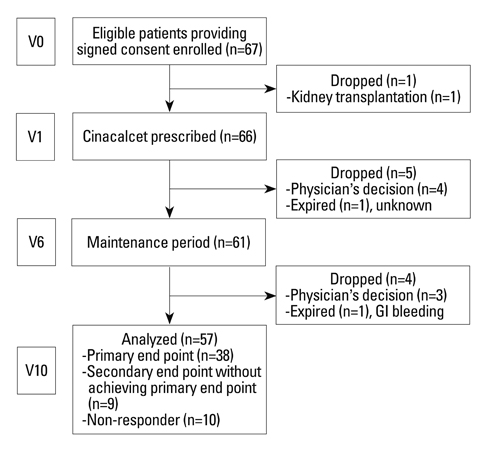
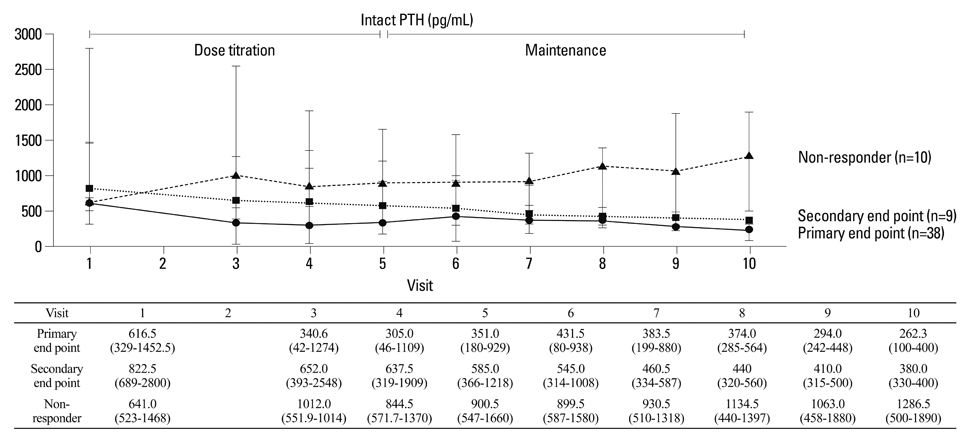
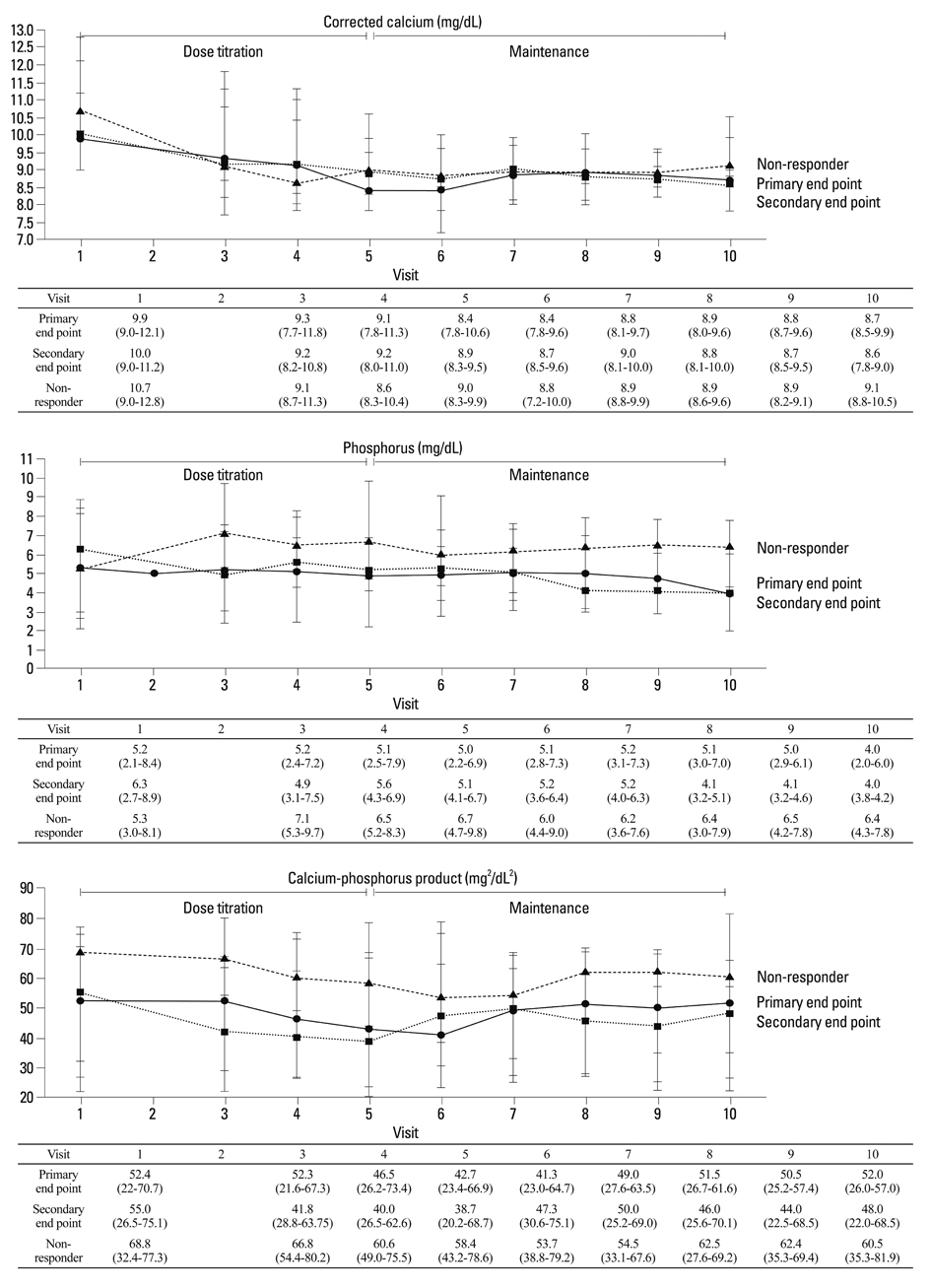
A prospective, single-arm, multi-center study was performed for 24 weeks. Cinacalcet was administered to patients with intact parathyroid hormone (iPTH) level greater than 300 pg/mL. Cinacalcet was started at a dose of 25 mg daily and titrated until 100 mg to achieve a serum iPTH level <300 pg/mL (primary end point). Early response to cinacalcet was defined as a decrease of iPTH more than 50% within one month.
RESULTS
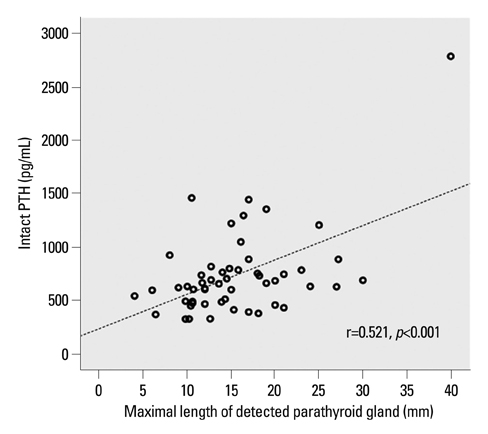
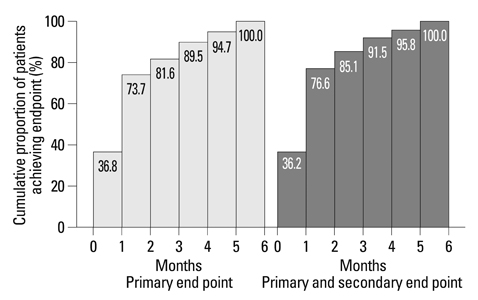
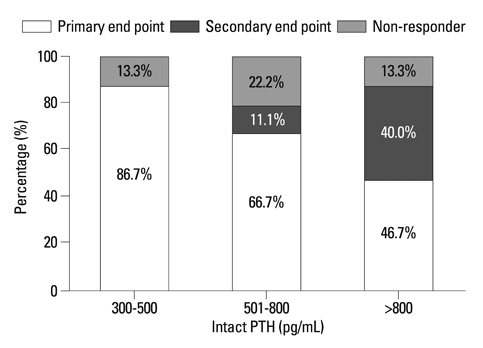
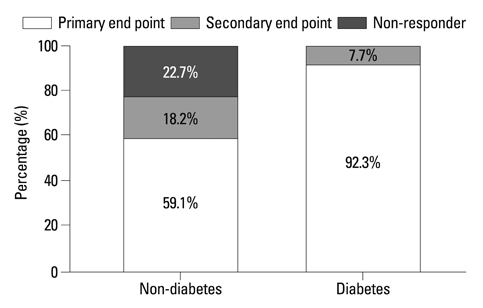
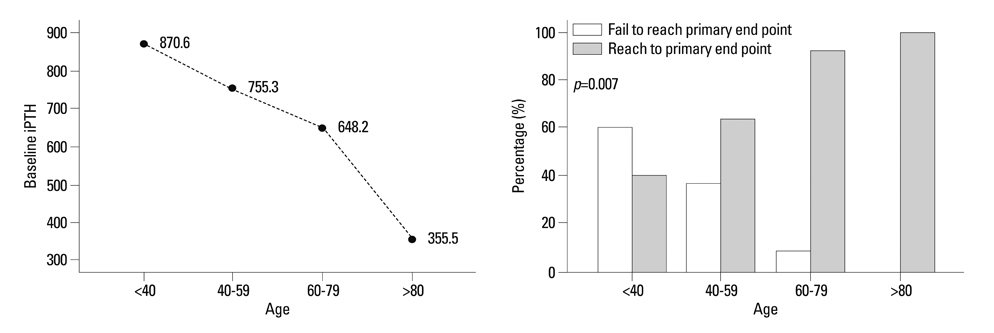
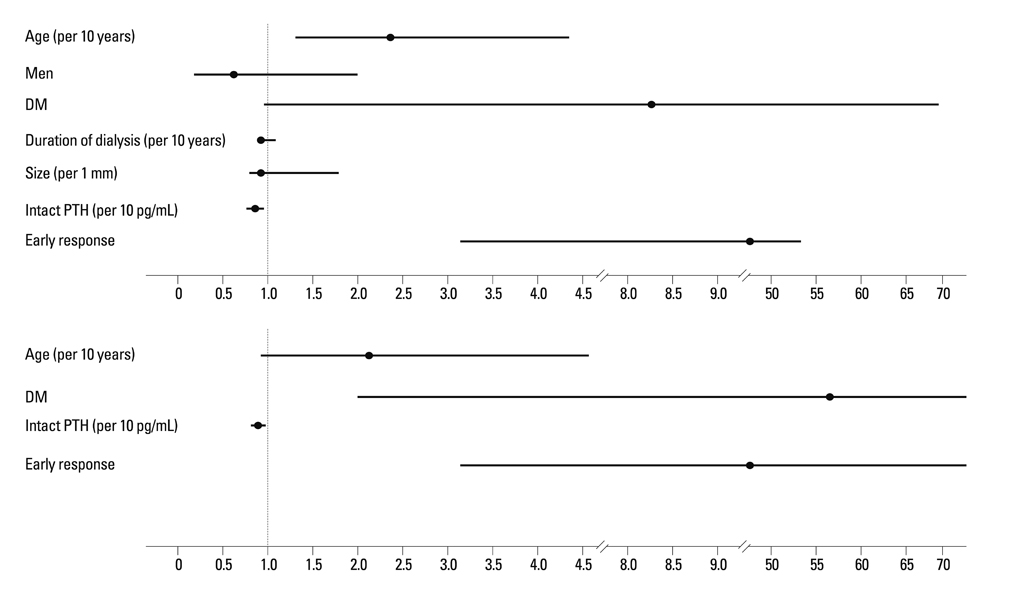
Fifty-seven patients were examined. Based on the magnitude of iPTH decrease, patients were divided into responder (n=47, 82.5%) and non-responder (n=10, 17.5%) groups. Among the responders, 38 achieved the primary end point, whereas 9 patients showed a reduction in serum iPTH of 30% or more, but did not reach the primary end point. Compared to non-responders, responders were significantly older (p=0.026), female (p=0.041), and diabetics (p<0.001). Additionally, early response was observed more frequently in the responders (30/47, 63.8%), of whom the majority (27/30, 90.0%) achieved the primary end point. Multivariate analysis showed that lower baseline iPTH levels [odds ratio (OR) 0.96, 95% confidence interval (CI) 0.93-0.99], the presence of diabetes (OR 46.45, CI 1.92-1125.6) and early response (OR 21.54, CI 2.94-157.7) were significant clinical factors affecting achievement of iPTH target.
CONCLUSION
Cinacalcet was effective in most hemodialysis patients with refractory SHPT. The presence of an early response was closely associated with the achievement of target levels of iPTH.
Keyword
MeSH Terms
Figure
Reference
-
1. Block GA, Zaun D, Smits G, Persky M, Brillhart S, Nieman K, et al. Cinacalcet hydrochloride treatment significantly improves all-cause and cardiovascular survival in a large cohort of hemodialysis patients. Kidney Int. 2010. 78:578–589.
Article2. Block GA, Martin KJ, de Francisco AL, Turner SA, Avram MM, Suranyi MG, et al. Cinacalcet for secondary hyperparathyroidism in patients receiving hemodialysis. N Engl J Med. 2004. 350:1516–1525.
Article3. Cozzolino M, Mazzaferro S, Messa P. New insights into the role of calcium-sensing receptor activation. J Nephrol. 2011. 24:Suppl 18. S38–S41.
Article4. Moe SM, Chertow GM, Coburn JW, Quarles LD, Goodman WG, Block GA, et al. Achieving NKF-K/DOQI bone metabolism and disease treatment goals with cinacalcet HCl. Kidney Int. 2005. 67:760–771.
Article5. Cunningham J, Danese M, Olson K, Klassen P, Chertow GM. Effects of the calcimimetic cinacalcet HCl on cardiovascular disease, fracture, and health-related quality of life in secondary hyperparathyroidism. Kidney Int. 2005. 68:1793–1800.
Article6. Drüeke TB, Ritz E. Treatment of secondary hyperparathyroidism in CKD patients with cinacalcet and/or vitamin D derivatives. Clin J Am Soc Nephrol. 2009. 4:234–241.
Article7. Kalantar-Zadeh K, Shah A, Duong U, Hechter RC, Dukkipati R, Kovesdy CP. Kidney bone disease and mortality in CKD: revisiting the role of vitamin D, calcimimetics, alkaline phosphatase, and minerals. Kidney Int Suppl. 2010. S10–S21.
Article8. Frazão JM, Messa P, Mellotte GJ, Geiger H, Hagen EC, Quarles LD, et al. Cinacalcet reduces plasma intact parathyroid hormone, serum phosphate and calcium levels in patients with secondary hyperparathyroidism irrespective of its severity. Clin Nephrol. 2011. 76:233–243.
Article9. Young EW, Akiba T, Albert JM, McCarthy JT, Kerr PG, Mendelssohn DC, et al. Magnitude and impact of abnormal mineral metabolism in hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis. 2004. 44:5 Suppl 2. 34–38.
Article10. Moe SM, Cunningham J, Bommer J, Adler S, Rosansky SJ, Urena-Torres P, et al. Long-term treatment of secondary hyperparathyroidism with the calcimimetic cinacalcet HCl. Nephrol Dial Transplant. 2005. 20:2186–2193.
Article11. Tentori F, Blayney MJ, Albert JM, Gillespie BW, Kerr PG, Bommer J, et al. Mortality risk for dialysis patients with different levels of serum calcium, phosphorus, and PTH: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis. 2008. 52:519–530.
Article12. Goodman WG, Frazao JM, Goodkin DA, Turner SA, Liu W, Coburn JW. A calcimimetic agent lowers plasma parathyroid hormone levels in patients with secondary hyperparathyroidism. Kidney Int. 2000. 58:436–445.
Article13. Lindberg JS, Culleton B, Wong G, Borah MF, Clark RV, Shapiro WB, et al. Cinacalcet HCl, an oral calcimimetic agent for the treatment of secondary hyperparathyroidism in hemodialysis and peritoneal dialysis: a randomized, double-blind, multicenter study. J Am Soc Nephrol. 2005. 16:800–807.
Article14. Akizawa T, Kido R, Fukagawa M, Onishi Y, Yamaguchi T, Hasegawa T, et al. Decreases in PTH in Japanese hemodialysis patients with secondary hyperparathyroidism: associations with changing practice patterns. Clin J Am Soc Nephrol. 2011. 6:2280–2288.
Article15. Lucchi L, Carboni C, Stipo L, Malaguti V, Ferrari F, Graziani R, et al. Early initiation of cinacalcet for the treatment of secondary hyperparathyroidism in hemodialysis patients: a three-year clinical experience. Artif Organs. 2011. 35:1186–1193.
Article16. Suzuki H, Inoue T, Watanabe Y, Kikuta T, Sato T, Tsuda M, et al. Does cinacalcet HCl, an oral calcimimetic agent for the treatment of secondary hyperparathyroidism, improve arterial stiffness in patients on continuous ambulatory peritoneal dialysis? Adv Perit Dial. 2011. 27:134–139.17. Battistella M, Richardson RM, Bargman JM, Chan CT. Improved parathyroid hormone control by cinacalcet is associated with reduction in darbepoetin requirement in patients with end-stage renal disease. Clin Nephrol. 2011. 76:99–103.
Article18. Wald R, Tentori F, Tighiouart H, Zager PG, Miskulin DC. Impact of the Kidney Disease Outcomes Quality Initiative (KDOQI) Clinical Practice Guidelines for Bone Metabolism and Disease in a large dialysis network. Am J Kidney Dis. 2007. 49:257–266.
Article19. National Kidney Foundation. K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003. 42:4 Suppl 3. S1–S201.20. Shoback DM, Bilezikian JP, Turner SA, McCary LC, Guo MD, Peacock M. The calcimimetic cinacalcet normalizes serum calcium in subjects with primary hyperparathyroidism. J Clin Endocrinol Metab. 2003. 88:5644–5649.
Article21. Kruse AE, Eisenberger U, Frey FJ, Mohaupt MG. Effect of cinacalcet cessation in renal transplant recipients with persistent hyperparathyroidism. Nephrol Dial Transplant. 2007. 22:2362–2365.
Article22. Komaba H, Nakanishi S, Fujimori A, Tanaka M, Shin J, Shibuya K, et al. Cinacalcet effectively reduces parathyroid hormone secretion and gland volume regardless of pretreatment gland size in patients with secondary hyperparathyroidism. Clin J Am Soc Nephrol. 2010. 5:2305–2314.
Article23. Yamamoto M, Ogata H, Mizobuchi M, Yoshida N, Kumata-Maeta C, Koiwa F, et al. Number of enlarged parathyroid glands might be a predictor of cinacalcet response in advanced secondary hyperparathyroidism. Clin Exp Nephrol. 2012. 16:292–299.
Article24. Segura Torres P, Borrego Utiel FJ, Sánchez Perales MC, García Cortés MJ, Biechy Baldán MM, Pérez Bañasco V. [Analysis of the efficacy and factors influencing the response of secondary hyperparathyroidism patients on hemodialysis to cinacalcet]. Nefrologia. 2010. 30:443–451.25. Pei Y, Hercz G, Greenwood C, Segre G, Manuel A, Saiphoo C, et al. Renal osteodystrophy in diabetic patients. Kidney Int. 1993. 44:159–164.
Article26. Vincenti F, Hattner R, Amend WJ Jr, Feduska NJ, Duca RM, Salvatierra O Jr. Decreased secondary hyperparathyroidism in diabetic patients receiving hemodialysis. JAMA. 1981. 245:930–933.
Article27. Vincenti F, Arnaud SB, Recker R, Genant H, Amend WJ Jr, Feduska NJ, et al. Parathyroid and bone response of the diabetic patient to uremia. Kidney Int. 1984. 25:677–682.
Article28. Dvorak MM, Riccardi D. Ca2+ as an extracellular signal in bone. Cell Calcium. 2004. 35:249–255.
Article29. Chang W, Tu C, Chen TH, Bikle D, Shoback D. The extracellular calcium-sensing receptor (CaSR) is a critical modulator of skeletal development. Sci Signal. 2008. 1:ra1.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Functional Parathyroid Cyst: A case report
- Disease of Parathyroid and Surgical Strategy
- Relation between the Protein Intake, and Serum Phosphorus and Parathyroid Hormone Levels in Hemodialysis Patients
- Long-term effectiveness of cinacalcet in non-dialysis patients with chronic kidney disease and secondary hyperparathyroidism
- A Studyof Dermal Mast Cells Number in End Stage of Renal Failure