J Korean Soc Spine Surg.
2013 Sep;20(3):86-91. 10.4184/jkss.2013.20.3.86.
Long Term Results of Vertebroplasty in the Treatment of Osteoporotic Compression Fracture
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Dong-A University, Korea. gylee@dau.ac.kr
- KMID: 1487973
- DOI: http://doi.org/10.4184/jkss.2013.20.3.86
Abstract
- STUDY DESIGN: A retrospective study.
OBJECTIVES
The purpose of this study was to assess the clinical efficacy and long term results of patients undergoing percutaneous vertebroplasty, with bone cement, for osteoporotic compression fractures. SUMMARY OF LITERATURE REVIEW: Percutaneous vertebroplasty is an effective surgical method for the treatment of osteoporotic compression fracture.
MATERIALS AND METHODS
Among 82 patients who underwent percutaneous vertebroplasty, with bone cement, between February 2005 and February 2008, 54 patients who were followed-up for more than 4 years were selected. We compared the postoperative clinical and radiological findings immediately and at 1, 2, and 4 year follow-up. Clinical findings were evaluated using the Visual analogue scale (VAS) score. Radiologically, height of the vertebral body and adjacent vertebral body fracture were also assessed.
RESULTS
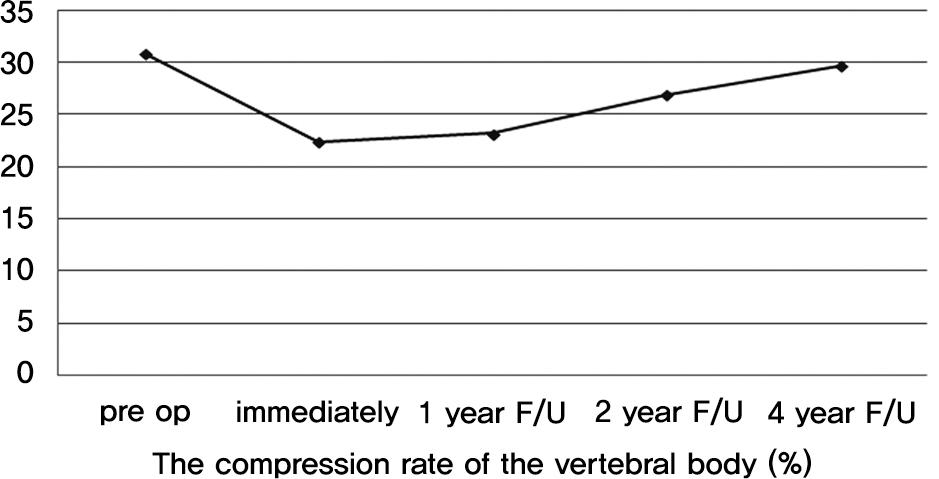
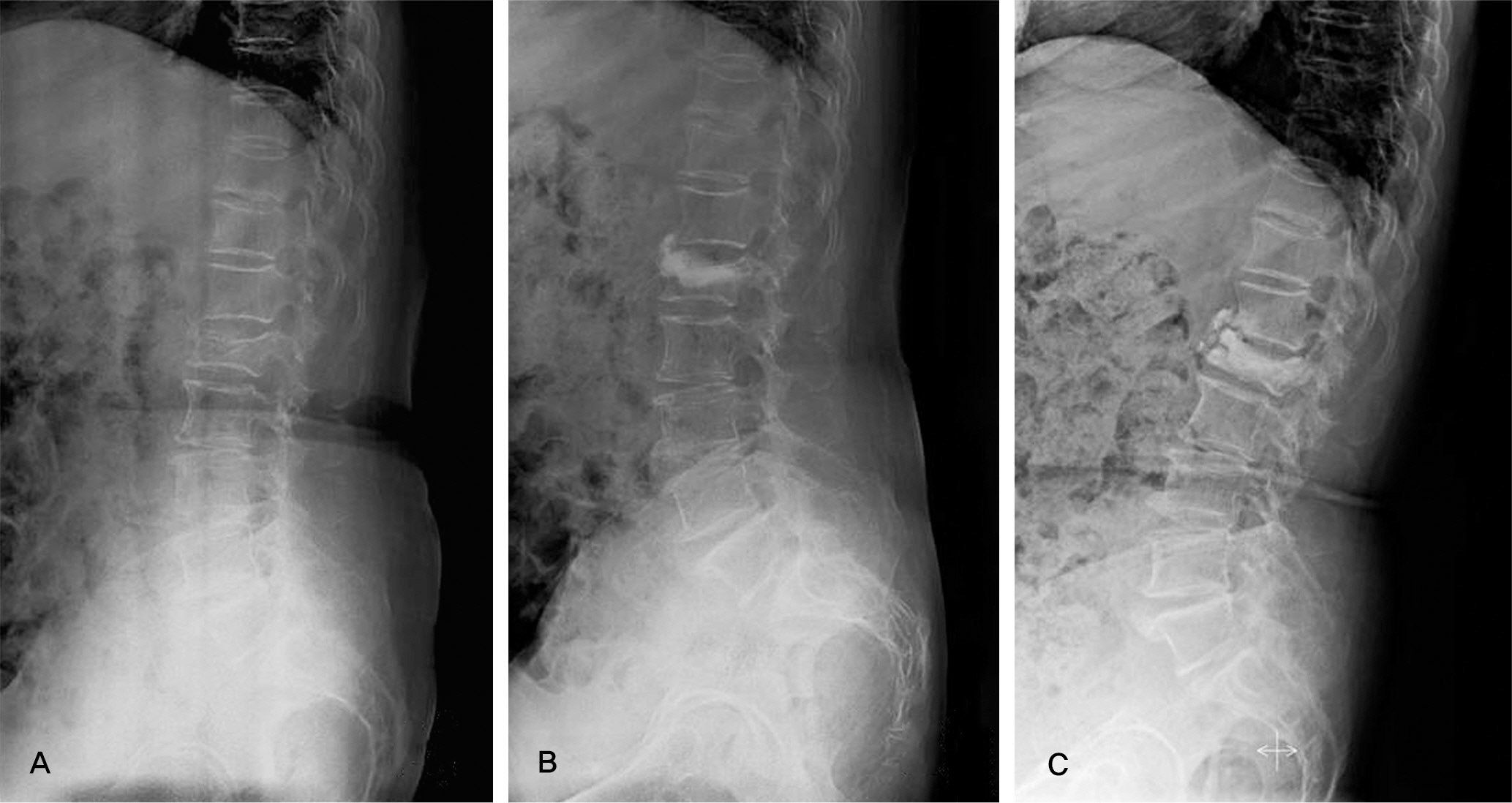
Clinical outcome by mean VAS score revealed a change from 5.9 to 3.8 points preoperatively. The mean VAS scores were 3.4, 3.5 and 3.7 at 1, 2, 4 year follow-up, retrospectively. The compression rate of the vertebral body on plain radiographs was 30.8% preoperatively, 22.4% immediately after the operation, 23.2% at 1 year follow-up, 26.9% at 2 year follow-up, and 29.7% at 4 year follow-up. A new adjacent vertebral body fracture was noted in 7 patients at 1 year follow-up and 3 patients at 2 and 4 year follow-up, respectively.
CONCLUSIONS
Percutaneous vertebroplasty is a valuable method for the treatment of osteoporotic compression fractures, providing immediate pain relief as well as long term pain relief. However, percutaneous vertebroplasty gave unsatisfactory report about height of the vertebral body and adjacent vertebral body fracture.
Keyword
MeSH Terms
Figure
Reference
-
1. Galibert P, Deramond H, Rosat P, Le Gars D. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie. 1987; 33:166–8.2. Barr JD, Barr MS, Lemley TJ, Mccann RM. Percutaneous vertebroplasty for pain relief and spinal stablization. Spine (Phila Pa 1976). 2000; 25:923–8.3. Deramond H, Depreister C, Galibert P, Le Gars D. Percutaneous vertebroplasty with polymethylmethacrylate; technique, indication, and results. Radiologic Clinics of North America. 1998; 36:533–46.4. Weill A, Chiras J, Simon JM, Rose M, Sola-Martinez T, Enkaoua E. Spinal metastasis: indications for and results of percutaneous injection of acrylic surgical cement. Radiology. 1996; 199:241–7.5. Lindsay R, Burge RT, Strauss DM. One year outcomes and costs following a vertebral fracture. Osteoporos Int. 2005; 16:78–85.
Article6. Perez-Higueras A, Alvarez L, Rossi RE, Quinones D, AlAssir I. Percutaneous vertebroplasty: longterm clinical and radiological outcome. Neroradiology. 2002; 44:950–4.7. Rockwood CA, Green DP, Bucholz RW. Rockwood and Green's fractures in adults. Vol. 3. 6th ed.Philadelphia, PA: Lippincott Williams & Wilkins;2006. p. 4–11.8. Tsai TT, Chen WJ, Lai PL, et al. Polymethylmethacrylate cement dislodgement following percutaneous vertebroplasty: a case report. Spine (Phila Pa 1976). 2003; 28:457–60.9. Heo DH, Chin DK, Yoon YS, Kuh SU. Recollapse of previous vertebral compression fracture after percutaneous vertebroplasty. Osteoporos Int. 2009; 20:473–80.
Article10. Kim WJ, Yeom JS, Kang JW, et al. Percutaneous vertebroplasty: short-term results of 38cases. J Korean Orthop Assoc. 2002; 37:471–7.11. Teng MM, Wei CJ, Wei LC. Kyphosis correction and height restoration effects of percutaneous vertebroplasty. AJNR Am J Neuroradiol. 2003; 24:1893–900.12. Mousavi P, Roth S, Finkelstein J, Cheung G, Whyne C. Volumetric quantification of cement leakage following percutaneous vertebroplasty in metastatic and osteoporotic vertebrae. Neurosurg. 2003; 99:56–9.
Article13. Shin KS, Kim JS, Lee DW. Surgical treatment of root injury after percutaneous vertebroplasty: case report. J Korean soc spine surg. 2002; 9:54–8.
Article14. Chiras J, Depriester C, Weill A, Sola-Martinez MT, Deramond H. Percutaneous vertebral surgery. Technics and indications. Neuroradiol. 1997; 24:45–59.15. Cortet B, Cotten A, Boutry N, et al. Percutaneous vertebroplasty in patients with osteolytic metastases or multiple myeloma. Rev Rhum Engl Ed. 1997; 64:177–83.16. Yeom JS, Kim WJ, Choy WS, Lee CK, Chang BS, Kang JW. Leakage of cement in percutaneous transpedicular vertebroplasty for painful osteoporotic compression fractures. J Bone Joint Surg. 2003; 85:83–9.
Article17. Jensen ME, Avery JE, Mathis JM, Kallmess DF, Cloft HJ, Dio JE. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fracture: technical aspects. Am J Neuroradiol. 1997; 18:1897–904.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vertebroplasty in the Multiple Osteoporotic Compression Fracture
- The effect of percutaneous vertebroplasty with bone cement in the treatment of osteoporotic thoracolumbar compression fracture
- Short-term Treatment Comparison of Teriparatide and Percutaneous Vertebroplasty in Patients with Acute Osteoporotic Vertebral Compression Fractures
- Percutaneous Vertebroplasty in Osteoporotic Vertebral Compression Fractures; The Degree of Vertebral Compression and Outcome
- Minimum 7 Years Follow-up of Percutaneous Vertebroplasty in Osteoporotic Compression Fracture