Korean J Radiol.
2013 Apr;14(2):366-374. 10.3348/kjr.2013.14.2.366.
Primary Endobronchial Marginal Zone B-Cell Lymphoma of Bronchus-Associated Lymphoid Tissue: CT Findings in 7 Patients
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Seoul 138-736, Korea. mimowdr@gmail.com
- 2Department of Pulmonary and Oncology Medicine, University of Ulsan College of Medicine, Seoul 138-736, Korea.
- 3Department of Pathology, University of Ulsan College of Medicine, Seoul 138-736, Korea.
- KMID: 1482801
- DOI: http://doi.org/10.3348/kjr.2013.14.2.366
Abstract
OBJECTIVE
To investigate CT and 18F-flurodeoxyglucose (18F-FDG) positron-emission tomography/CT findings of primary endobronchial marginal zone B-cell lymphoma of the bronchus-associated lymphoid tissue (BALT).
MATERIALS AND METHODS
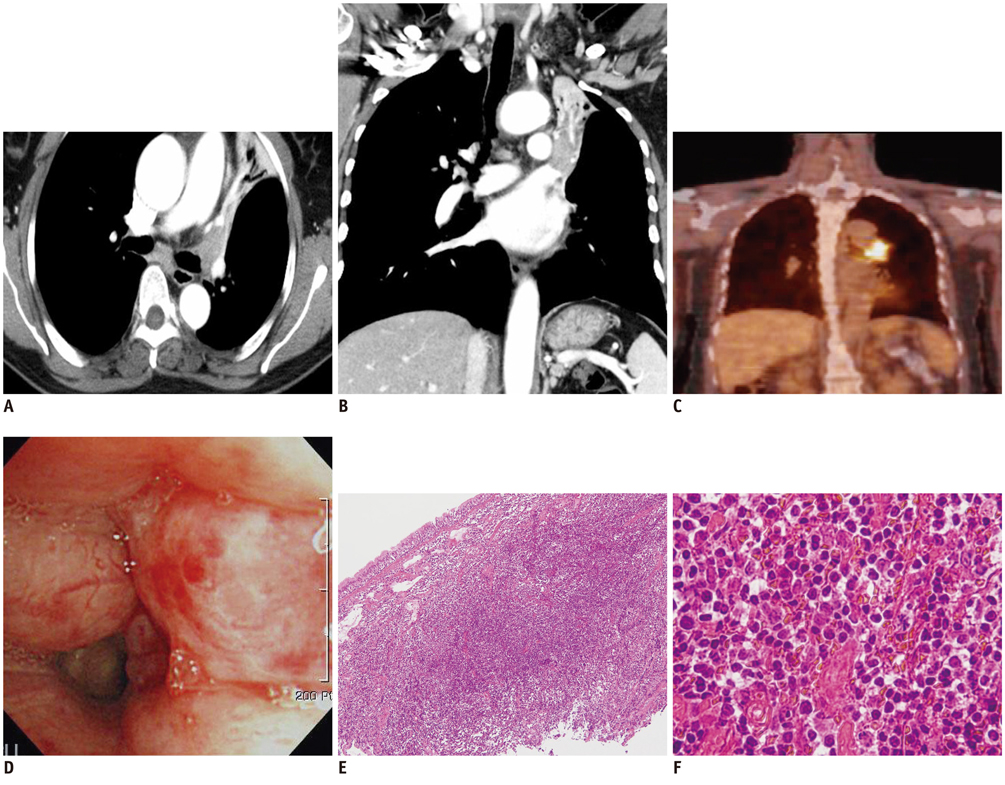
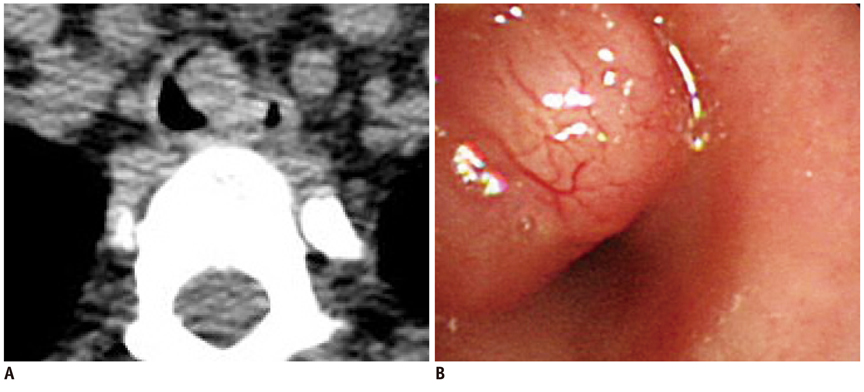
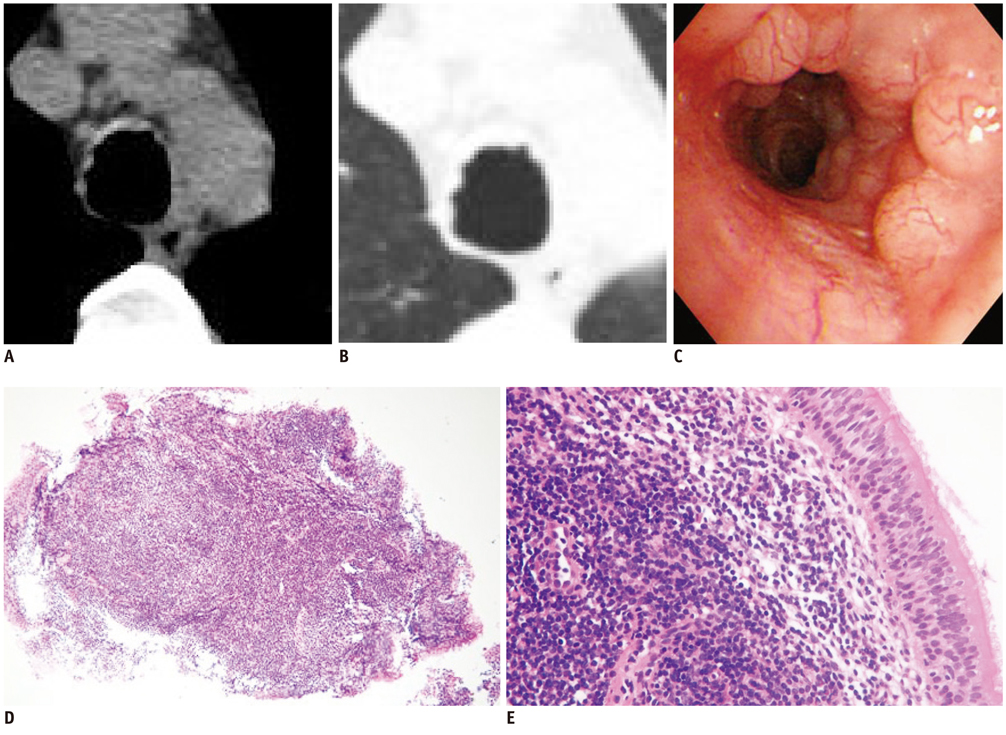
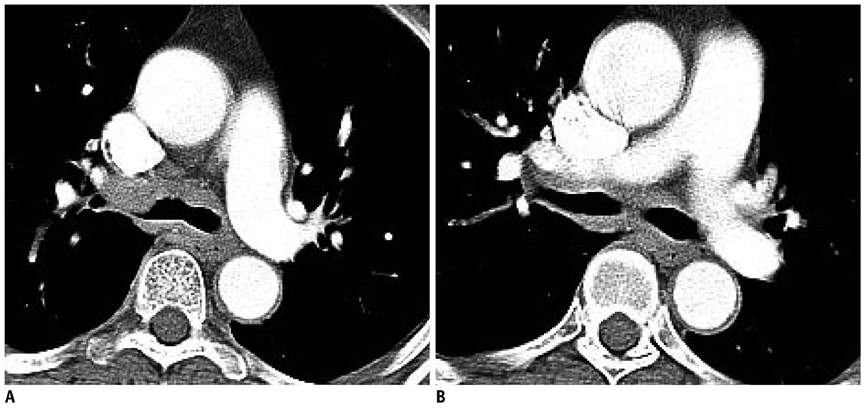
From June 2006 through April 2012, seven patients (six female, one male; age range, 21-61 years; mean age, 49 years) were examined who were pathologically diagnosed with the primary endobronchial marginal zone B-cell lymphoma of BALT. We evaluated the locations and characteristics of the lesions on CT and 18F-FDG-PET/CT scans. The lesions were classified into the following three patterns: 1) solitary intraluminal nodule; 2) several tiny nodular protrusions; and 3) diffuse wall thickening.
RESULTS
A solitary intraluminal nodule was observed in four patients (57.1%), several tiny nodular protrusion in two patients (28.6%), and diffuse wall thickening in one patient (14.3%). The lesions were categorized into 3 major locations: confined to the trachea (n = 3), confined to the lobar bronchus (n = 2), and diffuse involvement of the trachea and both main bronchi (n = 2). All lesions demonstrated homogeneous iso-attenuation as compared with muscle on pre- and post-enhancement scans. Secondary findings in the lungs (n = 3; 42.9%) included postobstructive lobar atelectasis (n = 1), air trapping (n = 1), and pneumonia (n = 1). On 18F-FDG-PET/CT (n = 5), 4 lesions showed homogeneous uptake with maximum standardized uptake values (mSUV), ranging 2.3-5.7 (mean mSUV: 3.3). One lesion showed little FDG uptake.
CONCLUSION
Primary endobronchial marginal zone B-cell lymphoma of the BALT manifests as three distinct patterns on CT, with the solitary intraluminal nodule presenting as the main pattern. Most lesions demonstrate homogeneous but weak FDG uptake on 18F-FDG-PET/CT.
Keyword
MeSH Terms
-
Adult
Biopsy
Bronchi/pathology
Female
Fluorodeoxyglucose F18/diagnostic use
Humans
Immunohistochemistry
Lymphoid Tissue/pathology
Lymphoma, B-Cell, Marginal Zone/pathology/*radiography/radionuclide imaging
Male
Middle Aged
Radiopharmaceuticals/diagnostic use
Retrospective Studies
Tomography, X-Ray Computed/*methods
Radiopharmaceuticals
Fluorodeoxyglucose F18
Figure
Cited by 1 articles
-
Squamous Cell Carcinomas of the Lung Which Presented as Numerous Polypoid Nodules in the Tracheobronchial Tree: A Case Report
Hyun Gyu Lee, Yo Won Choi, Hyun Jung Yoon, Seung Sam Paik
J Korean Soc Radiol. 2017;76(3):211-215. doi: 10.3348/jksr.2017.76.3.211.
Reference
-
1. McGuinness G, Scholes JV, Jagirdar JS, Lubat E, Leitman BS, Bhalla M, et al. Unusual lymphoproliferative disorders in nine adults with HIV or AIDS: CT and pathologic findings. Radiology. 1995. 197:59–65.2. Harris NL, Jaffe ES, Stein H, Banks PM, Chan JK, Cleary ML, et al. A revised European-American classification of lymphoid neoplasms: a proposal from the International Lymphoma Study Group. Blood. 1994. 84:1361–1392.3. Kinsely BL, Mastey LA, Mergo PJ, Voytovich MC, Zander D, Almasri NM, et al. Pulmonary mucosa-associated lymphoid tissue lymphoma: CT and pathologic findings. AJR Am J Roentgenol. 1999. 172:1321–1326.4. Li G, Hansmann ML, Zwingers T, Lennert K. Primary lymphomas of the lung: morphological, immunohistochemical and clinical features. Histopathology. 1990. 16:519–531.5. Ahmed S, Siddiqui AK, Rai KR. Low-grade B-cell bronchial associated lymphoid tissue (BALT) lymphoma. Cancer Invest. 2002. 20:1059–1068.6. Solomonov A, Zuckerman T, Goralnik L, Ben-Arieh Y, Rowe JM, Yigla M. Non-Hodgkin's lymphoma presenting as an endobronchial tumor: report of eight cases and literature review. Am J Hematol. 2008. 83:416–419.7. Hoffmann M, Kletter K, Diemling M, Becherer A, Pfeffel F, Petkov V, et al. Positron emission tomography with fluorine-18-2-fluoro-2-deoxy-D-glucose (F18-FDG) does not visualize extranodal B-cell lymphoma of the mucosa-associated lymphoid tissue (MALT)-type. Ann Oncol. 1999. 10:1185–1189.8. Hoffmann M, Kletter K, Becherer A, Jäger U, Chott A, Raderer M. 18F-fluorodeoxyglucose positron emission tomography (18F-FDG-PET) for staging and follow-up of marginal zone B-cell lymphoma. Oncology. 2003. 64:336–340.9. Beal KP, Yeung HW, Yahalom J. FDG-PET scanning for detection and staging of extranodal marginal zone lymphomas of the MALT type: a report of 42 cases. Ann Oncol. 2005. 16:473–480.10. Bae YA, Lee KS, Han J, Ko YH, Kim BT, Chung MJ, et al. Marginal zone B-cell lymphoma of bronchus-associated lymphoid tissue: imaging findings in 21 patients. Chest. 2008. 133:433–440.11. Shin CH, Paik SH, Park JS, Kim HK, Park SI, Cha JG, et al. Primary pulmonary T-cell lymphoma: a case report. Korean J Radiol. 2010. 11:234–238.12. Brandtzaeg P, Jahnsen FL, Farstad IN. Immune functions and immunopathology of the mucosa of the upper respiratory pathways. Acta Otolaryngol. 1996. 116:149–159.13. Tirouvanziam R, Khazaal I, N'Sondé V, Peyrat MA, Lim A, de Bentzmann S, et al. Ex vivo development of functional human lymph node and bronchus-associated lymphoid tissue. Blood. 2002. 99:2483–2489.14. Anaya JM, McGuff HS, Banks PM, Talal N. Clinicopathological factors relating malignant lymphoma with Sjögren's syndrome. Semin Arthritis Rheum. 1996. 25:337–346.15. Trédaniel J, Peillon I, Fermé C, Brice P, Gisselbrecht C, Hirsch A. Endobronchial presentation of Hodgkin's disease: a report of nine cases and review of the literature. Eur Respir J. 1994. 7:1852–1855.16. Berkman N, Lafair J, Okon E, Polliack A. Obstructive solitary bronchial non-Hodgkin's lymphoma--a rare presentation of primary extranodal disease. Leuk Lymphoma. 1992. 8:405–407.17. McRae WM, Wong CS, Jeffery GM. Endobronchial non-Hodgkin's lymphoma. Respir Med. 1998. 92:975–977.18. Hashemi SM, Heitbrink MA, Jiwa M, Boersma WG. A patient with endobronchial BALT lymphoma successfully treated with radiotherapy. Respir Med. 2007. 101:2227–2229.19. Erbaycu AE, Karasu I, Ozdemirkiran FG, Yücel N, Ozsöz A, Bilgir O. Endobronchial low-grade MALT lymphoma causing unilateral hypertranslucency. Monaldi Arch Chest Dis. 2004. 61:237–240.20. Kang JY, Park HJ, Lee KY, Lee SY, Kim SJ, Park SH, et al. Extranodal marginal zone lymphoma occurring along the trachea and central airway. Yonsei Med J. 2008. 49:860–863.21. Nathwani BN, Anderson JR, Armitage JO, Cavalli F, Diebold J, Drachenberg MR, et al. Marginal zone B-cell lymphoma: a clinical comparison of nodal and mucosa-associated lymphoid tissue types. Non-Hodgkin's Lymphoma Classification Project. J Clin Oncol. 1999. 17:2486–2492.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Primary Nodal Type Marginal Zone B-Cell Lymphoma of the Intra-Parotid Lymph Node Mistaken to Primary Benign Parotid Mass
- A Case of Primary Pulmonary Extranodal Marginal Zone B-Cell Lymphoma of the MALT Type
- A Case of Synchronous Lung Adenocarcinoma and Extranodal Marginal Zone B-Cell Lymphoma of Mucosa-Associated Lymphoid Tissue (MALT) Type
- Role of Chemotherapy in Gastric Marginal Zone B-Cell Lymphoma of Mucosa-Associated Lymphoid Tissue (MALT) Type
- A Case of Primary Cutaneous Marginal Zone B-cell Lymphoma