J Korean Soc Radiol.
2010 Apr;62(4):343-349. 10.3348/jksr.2010.62.4.343.
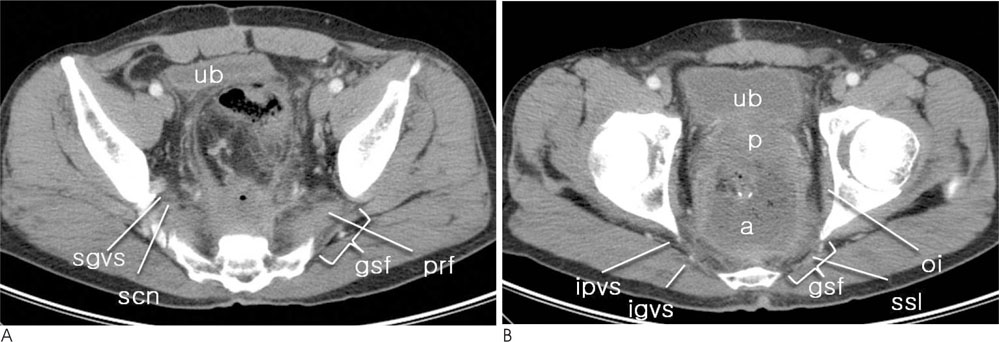
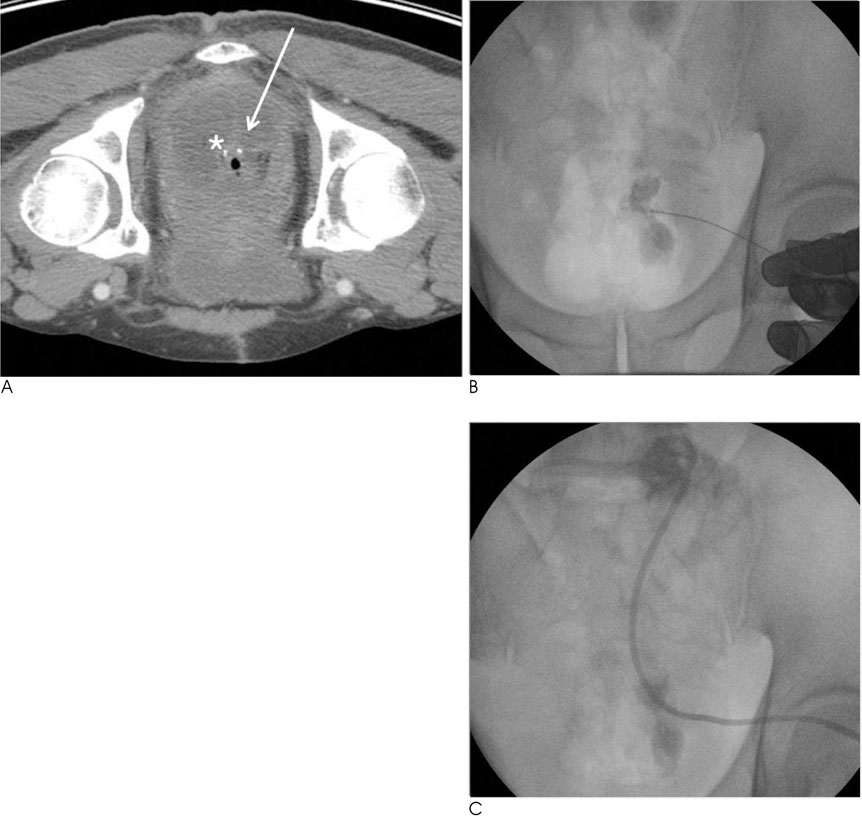
Percutaneous Drainage of Postoperative Pelvic Abscess: Fluoroscopic and US-Guided Transgluteal Approach
- Affiliations
-
- 1Department of Radiology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Korea. summerson@paran.com
- 2Department of Radiology, Kangwon National University College of Medicine, Korea.
- KMID: 1460066
- DOI: http://doi.org/10.3348/jksr.2010.62.4.343
Abstract
- PURPOSE
To retrospectively review the effectiveness and safety of fluoroscopic and US-guided percutaneous transgluteal drainage of postoperative pelvic abscesses.
MATERIALS AND METHODS
From January 2002 to December 2007, 594 patients underwent surgery at our institution due to rectosigmoid cancer. A retrospective analysis revealed that percutaneous drainage of a postoperative pelvic abscess was performed in 19 out of the 594 patients (3.19%) that underwent surgery (13 male, 6 female; mean age, 57.9 years; age range, 40-82 years). The transgluteal and other methods were used for percutaneous drainage and the success rate, duration of therapy, and complication rate were evaluated.
RESULTS
The transgluteal approach was performed with fluoroscopic and US-guidance in 10 patients (52.6%). A catheter was inserted through a preexisting surgical drain in 5 patients (26.3%). The transabdominal approach was performed under US-guidance in 4 patients (21.0%). Technical success was achieved in all patients. The catheter was removed after a mean of 14 days. In 2 patients, who were treated by the transgluteal apporoach, subsequent surgery was performed due to incomplete resolution of the abscess (10.5%). The mean duration of catheter drainage using the transgluteal approach (16.5 days) was longer than other methods (11.2 days). Furthermore, no procedure-related major complications or mortality was observed in all methods.
CONCLUSION
The percutaneous transgluteal approach to a postoperative pelvic abscess with US and fluoroscopic guidance is relatively safe and effective.
Figure
Reference
-
1. Welch CE, Malt RA. Abdominal surgery (first of three parts). N Engl J Med. 1983; 308:624–632.2. Welch CE, Malt RA. Abdominal surgery (second of three parts). N Engl J Med. 1983; 308:685–695.3. Welch CE, Malt RA. Abdominal surgery (third of three parts). N Engl J Med. 1983; 308:753–760.4. Varghese JC, O'Neill MJ, Gervais DA, Boland GW, Mueller PR. Transvaginal catheter drainage of tuboovarian abscess using the trocar method: technique and literature review. AJR Am J Roentgenol. 2001; 177:139–144.5. Gazelle GS, Haaga JR, Stellato TA, Gauderer MW, Plecha DT. Pelvic abscesses: CT-guided transrectal drainage. Radiology. 1991; 181:49–51.6. Pereira JK, Chait PG, Miller SF. Deep pelvic abscesses in children: transrectal drainage under radiologic guidance. Radiology. 1996; 198:393–396.7. Whelan MA, Gold RP. Computed tomography of the sacrum: 1. Normal anatomy. AJR Am J Roentgenol. 1982; 139:1183–1190.8. Whelan MA, Hilal SK, Gold RP, Luken MG, Michelson WJ. Computed tomography of the sacrum: 2. Pathology. AJR Am J Roentgenol. 1982; 139:1191–1195.9. Wechsler RJ, Schilling JF. CT of the gluteal region. AJR Am J Roentgenol. 1985; 144:185–190.10. Federle MP, Moss AA, Margolin FR. Role of computed tomography in patients with "Sciatica". J Comput Assist Tomogr. 1980; 4:335–341.11. Butch RJ, Mueller PR, Ferrucci JT, Wittenberg J, Simeone JF, White EM, et al. Drainage of pelvic abscesses through the greater sciatic foramen. Radiology. 1986; 158:487–491.12. Harisinghani MG, Gervais DA, Maher MM, Cho CH, Hahn PF, Varghese J, et al. Transgluteal approach for percutaneous drainage of deep pelvic abscesses: 154 cases. Radiology. 2003; 228:701–705.13. Walser E, Raza S, Hernandez A, Ozkan O, Kathuria M, Akinci D. Sonographically guided transgluteal drainage of pelvic abscesses. AJR Am J Roentgenol. 2003; 181:498–500.14. Cahill AM, Baskin KM, Kaye RD, Fitz CR, Towbin RB. Transgluteal approach for draining pelvic fluid collections in pediatric patients. Radiology. 2005; 234:893–898.15. Gervais DA, Hahn PF, O'Neill MJ, Mueller PR. CT-guided transgluteal drainage of deep pelvic abscesses in children: selective use as an alternative to transrectal drainage. AJR Am J Roentgenol. 2000; 175:1393–1396.16. Gervais DA, Ho CH, O'Neill MJ, Arellano RS, Hahn PF, Mueller PR. Recurrent abdominal and pelvic abscesses: incidence, results of repeated percutaneous drainage, and underlying causes in 956 drainages. AJR Am J Roentgenol. 2004; 182:463–466.17. Maher MM, Gervais DA, Kalra MK, Lucey B, Sahani DV, Arellano R, et al. The inaccessible or undrainable abscess: how to drain it. Radiographics. 2004; 24:717–735.18. Gervais DA, Brown SD, Connolly SA, Brec SL, Harisinghani MG, Mueller PR. Percutaneous imaging-guided abdominal and pelvic abscess drainage in children. Radiographics. 2004; 24:737–754.19. Woo JK, Millward SF. Transgluteal approach for percutaneous drainage of deep pelvic abscesses: how to avoid injury to vital structures. Radiology. 2004; 233:300–301.20. Harisinghani MG, Gervais DA, Hahn PF, Cho CH, Jhaveri K, Varghese J, et al. CT-guided transgluteal drainage of deep pelvic abscesses: indications, technique, procedure-related complications, and clinical outcome. Radiographics. 2002; 22:1353–1367.21. Gupta S, Nguyen HL, Morello FA, Ahrar K, Wallace MJ, Madoff DC, et al. Various approaches for CT-guided percutaneous biopsy of deep pelvic lesions: anatomic and technical considerations. Radiographics. 2004; 24:175–189.22. Ryan JM, Murphy BL, Boland GW, Mueller PR. Use of the transgluteal route for percutaneous abscess drainage in acute diverticulitis to facilitate delayed surgical repair. AJR Am J Roentgenol. 1998; 170:1189–1193.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Drainage of Pelvic Fluid Collection
- Percutaneous Transgluteal Drainage of Seminal Vesicle Abscess
- Effectiveness of Fluoroscopic and US - Guided Percutaneous Catheter Drainage for Iliopsoas Abscess through the Anterolateral Transabdominal Approach
- Transrectal Drainage of Deep Pelvic Abscesses
- Endoscopic ultrasound-guided drainage for an abscess cavity