J Korean Soc Spine Surg.
2011 Dec;18(4):208-216. 10.4184/jkss.2011.18.4.208.
Comparative Study of the Clinical Outcomes of Unilateral Transforaminal Lumbar Interbody Fusion(TLIF) with Bilateral TLIF using Wiltse Approach and Conventional Approach
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Kyung Hee University, Korea.
- 2Department of medicine, Graduate School, Kyung Hee University, Korea. esson75@hanmail.net
- KMID: 1447998
- DOI: http://doi.org/10.4184/jkss.2011.18.4.208
Abstract
- STUDY DESIGN: Comparative study.
OBJECTIVES
To compare the outcomes of unilateral TLIF, bilateral TLIF using Wiltse approach and bilateral TLIF using conventional midline approach. SUMMARY OF LITERATURE REVIEW: There are many studies about outcomes of Unilateral TLIF, but few have compared the 3 different fusion procedures.
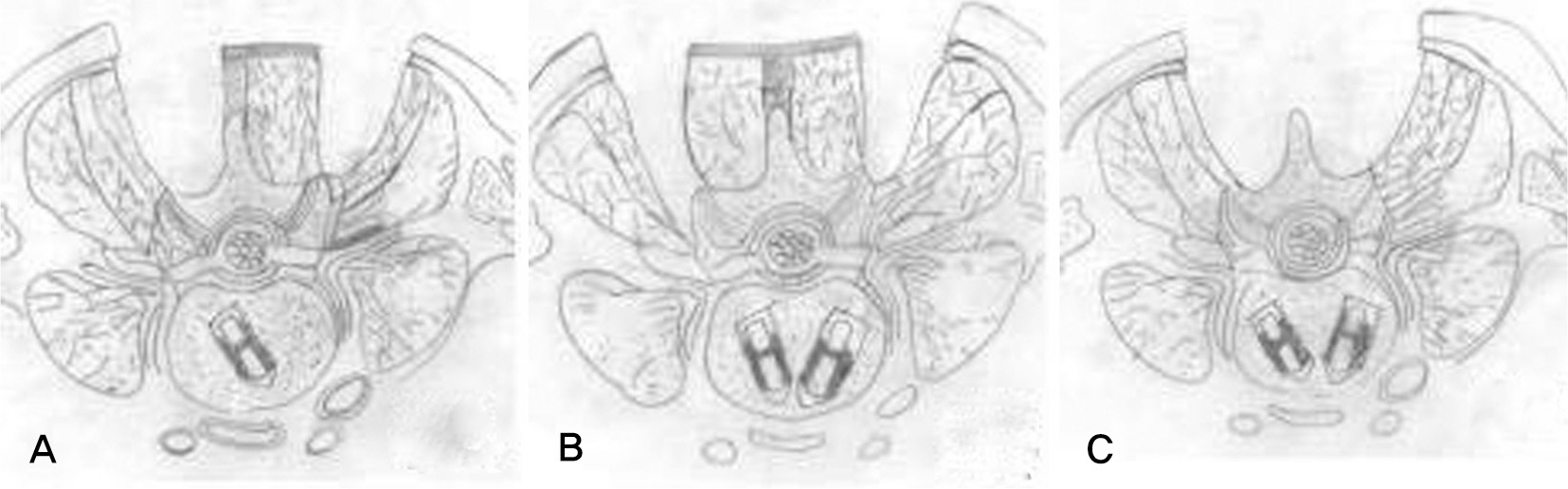
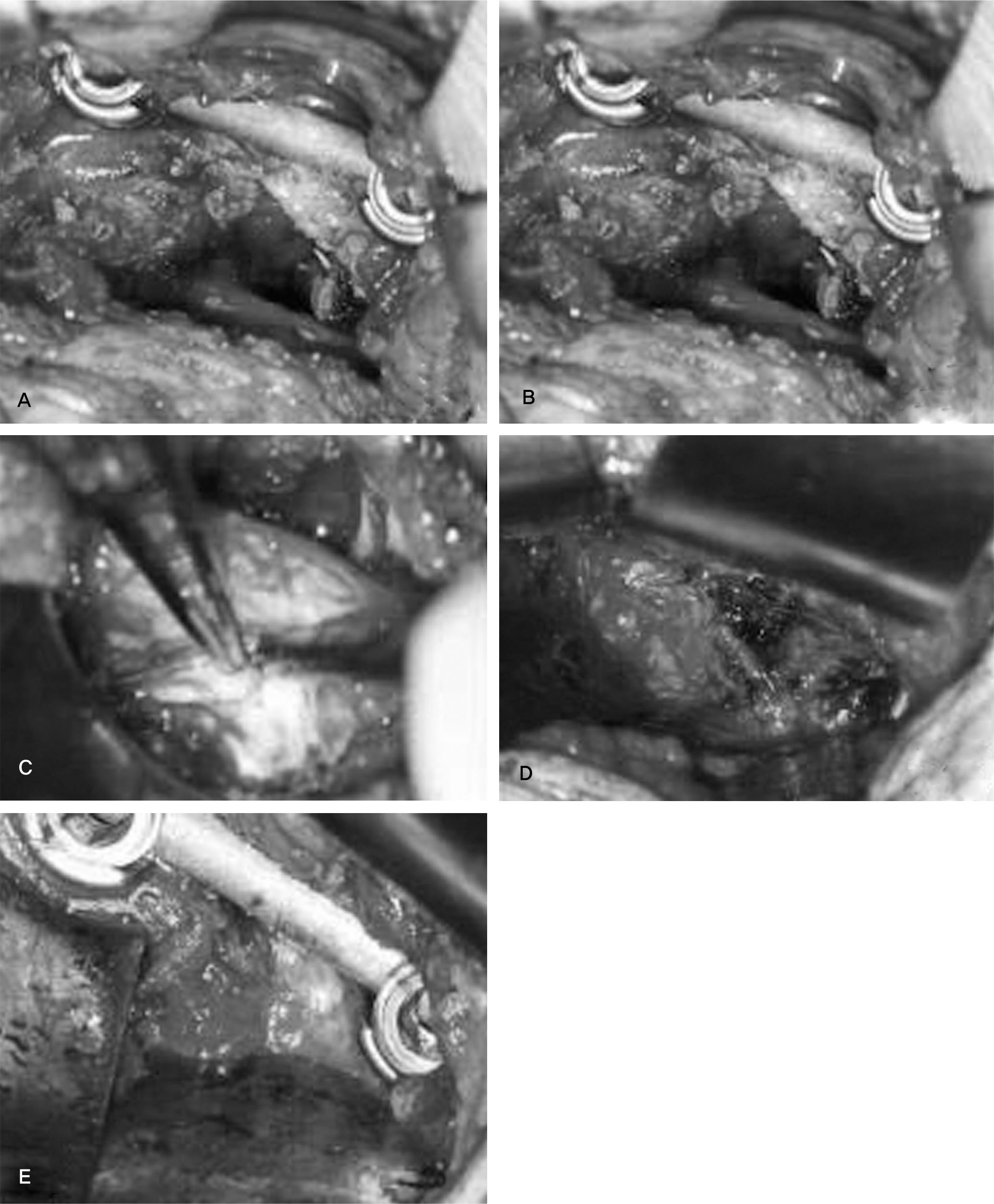
MATERIALS AND METHODS
60 patients were divided into 3 groups. Each group has enrolled 20 patients (Study group: unilateral TLIF, Control group 1: bilateral TLIF using Wiltse approach, Control group 2: bilateral TLIF using conventional midline approach). For clinical outcomes, we compared operative time, blood loss, time for ambulation and discharge, VAS for back pain and leg pain and ODI among three groups. For radiologic evaluation, disc height and segmental lordosis were examined.
RESULTS
The mean operative time was 147 minutes in study group(SG), 172 minutes in control group 1(CG1), 167 minutes in control group 2(CG2). The mean total blood loss was 466ml in SG, 569ml in CG1, 1140ml in CG2 respectively. VAS for back pain at the third postoperative day significantly decreased in SG and CG1 compared with CG2. There was no significant difference in ODI, disc height and segmental lordosis among the groups.
CONCLUSION
Using Wiltse approach, there were several advantages in decreasing blood loss, immediate postoperative back pain, hospital stay and early ambulation. Clinical and radiological results of unilateral TLIF were comparable with bilateral TLIF.
Figure
Reference
-
1. Sihvonen T, Herno A, Paljarva L, Airaksinen O, Partanen J, Tapaninaho A. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine (Phila Pa 1976). 1993; 18:575–81.
Article2. Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine (Phila Pa 1976). 2003; 28(15 Suppl):S26–35.
Article3. Holly LT, Schwender JD, Rouben DP, Foley KT. Minimally invasive transforaminal lumar inerbody fusion: indications, technique, and complications. Neurosurg Focus. 2006; 20:E6.4. Shunwu F, Xing Z, Fengdong Z, Xiangqian F. Minimally invasive transforaminal lumbar interbody fusion for the treatment of degenerative lumbar diseases. Spine (Phila Pa 1976). 2010; 35:1615–20.
Article5. Harms JG, Jeszenszky D. [In Process Citation]. Oper Orthop Traumatol. 1998; 10:90–102.6. Kim KT, Suk KS, Lee YH, Kim YW, Lee SH. The Posterior Decompression and Posterior Lumbar Interbody Fusion Using a Mini-open Technique – New Suggestion of Minimally Invasive Technique – A Prelimainary Report. J Korean Orthop Assoc. 2003; 38:492–7.7. Kim KT, Lee SH, Lee YH, Bae SC, Suk KS. Clinical outcomes of 3 fusion methods through the posterior approach in the lumbar spine. Spine (Phila Pa 1976). 2006; 31:1351–7.
Article8. Humphreys SC, Hodges SD, Patwardhan AG, Eck JC, Murphy RB, Covington LA. Comparison of posterior and transforaminal approaches to lumbar interbody fusion. Spine (Phila Pa 1976). 2001; 26:567–71.9. Lowe TG, Tahernia AD. Unilateral transforaminal posterior lumbar interbody fusion. Clin Orthop Relat Res. 2002; 394:64–72.
Article10. Isaacs RE, Podichetty VK, Santiago P, et al. Minimally invasive microendoscopy-assisted transforaminal lumbar interbody fusion wit instrumentation. J Neurosurg Spine. 2005; 3:98–105.11. Jang JS, Lee SH. Minimally invasive transforaminal lumbar interbody fusion with ipsilateral pedicle screw and contralateral facet screw fixation. J Neurosurg Spine. 2005; 3:218–23.
Article12. Mummaneni PV, Rodts GE Jr. The mini-open transforaminal lumbar interbody fusion. Neurosurgery. 2005; 57(4 Suppl):256–61.
Article13. Ozgur BM, Yoo K, Rodriguez G, Taylor WR. Minimally-invasive technique for transforaminal lumbar interbody fusion (TLIF). Eur Spine J. 2005; 14:887–94.
Article14. Schwender JD, Holly LT, Rouben DP, Foley KT. Minimally invasive transforaminal limbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech. 2005; 18 Suppl:S1–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Can Unilateral Minimally Invasive Transforaminal Lumbar Interbody Fusion (MIS TLIF) Result in Sufficient Reduction in Spondylolisthesis?: A Comparison with Open TLIF and Bilateral MIS TLIF
- Mini-invasive unilateral transforaminal lumbar interbody fusion and pedicle screw fixation
- Technique of Biportal Endoscopic Transforaminal Lumbar Interbody Fusion
- Short-Term Results of Transforaminal Lumbar Interbody Fusion Using Pedicle Screw with Cortical Bone Trajectory Compared with Conventional Trajectory
- Minimal Invasive Unilateral Transforaminal Lumbar Interbody Fusion by Sublaminar Decompression: Comparison to Bilateral Approach