J Korean Surg Soc.
2011 Oct;81(4):250-256. 10.4174/jkss.2011.81.4.250.
Role of transduodenal ampullectomy for tumors of the ampulla of Vater
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. pancreas@skku.edu
- 2Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1445745
- DOI: http://doi.org/10.4174/jkss.2011.81.4.250
Abstract
- PURPOSE
Tumors arising from the ampulla of Vater can be benign or malignant. Recently, endoscopic papillectomy has been employed in the management of benign ampulla of Vater tumors; however, surgical resection is the treatment of choice. The aim of this study was to define indications and suggest a role for transduodenal ampullectomy in the management of ampulla of Vater tumors.
METHODS
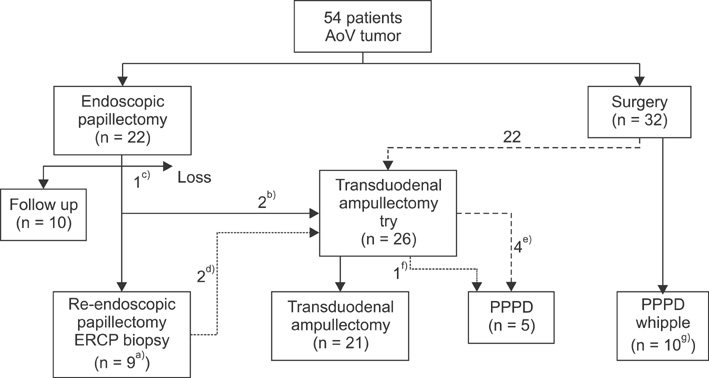
We retrospectively reviewed the medical records of 54 patients treated for ampulla of Vater tumors between January 1999 and December 2008.
RESULTS
Twenty-two endoscopic papillectomies and 21 transduodenal ampullectomies were performed. Four patients underwent transduodenal ampullectomy after endoscopic papillectomy due to a recurrent or remnant tumor. Recurrence or a remnant tumor was found in one patient after transduodenal ampullectomy compared to six patients after endoscopic papillectomy. Immediate intraoperative conversion from transduodenal ampullectomy to pancreaticoduodenectomy was performed in five patients based on intraoperative frozen biopsy analysis.
CONCLUSION
Transduodenal ampullectomy should be performed to treat ampulla of Vater tumors that are unsuitable for endoscopic papillectomy. Transduodenal ampullectomy can serve as an intermediate treatment option between endoscopic papillectomy and pancreaticoduodenectomy in the management of ampulla of Vater tumors.
MeSH Terms
Figure
Cited by 2 articles
-
Robotic transduodenal ampullectomy: Case report and review of the literature
Yun Le Linn, Zhongkai Wang, Brian K. P. Goh
Ann Hepatobiliary Pancreat Surg. 2021;25(1):150-154. doi: 10.14701/ahbps.2021.25.1.150.Transduodenal ampullectomy for ampullary tumors – single center experience of consecutive 26 patients
Sarang Hong, Ki Byung Song, Young-Joo Lee, Kwang-Min Park, Song Cheol Kim, Dae Wook Hwang, Jae Hoon Lee, Sang Hyun Shin, Jaewoo Kwon, Chung Hyeun Ma, Seunghyun Hwang, Guisuk Park, Yejong Park, Seung Jae Lee, Yong Woon Kim
Ann Surg Treat Res. 2018;95(1):22-28. doi: 10.4174/astr.2018.95.1.22.
Reference
-
1. Catalano MF, Linder JD, Chak A, Sivak MV Jr, Raijman I, Geenen JE, et al. Endoscopic management of adenoma of the major duodenal papilla. Gastrointest Endosc. 2004. 59:225–232.2. Charton JP, Deinert K, Schumacher B, Neuhaus H. Endoscopic resection for neoplastic diseases of the papilla of Vater. J Hepatobiliary Pancreat Surg. 2004. 11:245–251.3. Cheng CL, Sherman S, Fogel EL, McHenry L, Watkins JL, Fukushima T, et al. Endoscopic snare papillectomy for tumors of the duodenal papillae. Gastrointest Endosc. 2004. 60:757–764.4. Yoon SM, Kim MH, Kim MJ, Jang SJ, Lee TY, Kwon S, et al. Focal early stage cancer in ampullary adenoma: surgery or endoscopic papillectomy? Gastrointest Endosc. 2007. 66:701–707.5. Lee SY, Jang KT, Lee KT, Lee JK, Choi SH, Heo JS, et al. Can endoscopic resection be applied for early stage ampulla of Vater cancer? Gastrointest Endosc. 2006. 63:783–788.6. Kobayashi A, Konishi M, Nakagohri T, Takahashi S, Kinoshita T. Therapeutic approach to tumors of the ampulla of Vater. Am J Surg. 2006. 192:161–164.7. Yoon YS, Kim SW, Park SJ, Lee HS, Jang JY, Choi MG, et al. Clinicopathologic analysis of early ampullary cancers with a focus on the feasibility of ampullectomy. Ann Surg. 2005. 242:92–100.8. Halsted WS. Contributions to the surgery of the bile passages, especially of the common bile duct. Boston Med Surg J. 1899. 141:645–654.9. Whipple AO, Parsons WB, Mullins CR. Treatment of carcinoma of the ampulla of Vater. Ann Surg. 1935. 102:763–779.10. Winter JM, Cameron JL, Olino K, Herman JM, de Jong MC, Hruban RH, et al. Clinicopathologic analysis of ampullary neoplasms in 450 patients: implications for surgical strategy and long-term prognosis. J Gastrointest Surg. 2010. 14:379–387.11. Fraguela Mariña JA. Transduodenal ampullectomy in the treatment of villous adenomas and adenocarcinomas of the Vater's ampulla. Rev Esp Enferm Dig. 2004. 96:829–834.12. Dixon E, Vollmer CM Jr, Sahajpal A, Cattral MS, Grant DR, Taylor BR, et al. Transduodenal resection of peri-ampullary lesions. World J Surg. 2005. 29:649–652.13. Demetriades H, Zacharakis E, Kirou I, Pramateftakis MG, Sapidis N, Kanellos I, et al. Local excision as a treatment for tumors of ampulla of Vater. World J Surg Oncol. 2006. 4:14.14. Grobmyer SR, Stasik CN, Draganov P, Hemming AW, Dixon LR, Vogel SB, et al. Contemporary results with ampullectomy for 29 "benign" neoplasms of the ampulla. J Am Coll Surg. 2008. 206:466–471.15. Irani S, Arai A, Ayub K, Biehl T, Brandabur JJ, Dorer R, et al. Papillectomy for ampullary neoplasm: results of a single referral center over a 10-year period. Gastrointest Endosc. 2009. 70:923–932.16. Meneghetti AT, Safadi B, Stewart L, Way LW. Local resection of ampullary tumors. J Gastrointest Surg. 2005. 9:1300–1306.17. Maithel SK, Fong Y. Technical aspects of performing transduodenal ampullectomy. J Gastrointest Surg. 2008. 12:1582–1585.18. Park JS, Yoon DS, Park YN, Lee WJ, Chi HS, Kim BR. Transduodenal local resection for low risk group ampulla of Vater cancer patients. J Korean Surg Soc. 2004. 66:404–408.19. Böttger TC, Junginger T. Factors influencing morbidity and mortality after pancreaticoduodenectomy: critical analysis of 221 resections. World J Surg. 1999. 23:164–171.20. Bakkevold KE, Kambestad B. Morbidity and mortality after radical and palliative pancreatic cancer surgery. Risk factors influencing the short-term results. Ann Surg. 1993. 217:356–368.21. Seewald S, Omar S, Soehendra N. Endoscopic resection of tumors of the ampulla of Vater: how far up and how deep down can we go? Gastrointest Endosc. 2006. 63:789–791.22. Han J, Kim MH. Endoscopic papillectomy for adenomas of the major duodenal papilla (with video). Gastrointest Endosc. 2006. 63:292–301.23. Beger HG, Staib L, Schoenberg MH. Ampullectomy for adenoma of the papilla and ampulla of Vater. Langenbecks Arch Surg. 1998. 383:190–193.24. Branum GD, Pappas TN, Meyers WC. The management of tumors of the ampulla of Vater by local resection. Ann Surg. 1996. 224:621–627.25. Posner S, Colletti L, Knol J, Mulholland M, Eckhauser F. Safety and long-term efficacy of transduodenal excision for tumors of the ampulla of Vater. Surgery. 2000. 128:694–701.26. Clary BM, Tyler DS, Dematos P, Gottfried M, Pappas TN. Local ampullary resection with careful intraoperative frozen section evaluation for presumed benign ampullary neoplasms. Surgery. 2000. 127:628–633.27. Kim JW, Hwang YJ, Kim YI, Yun YK. Transduodenal ampullectomy in ampullary neoplasm. J Korean Surg Soc. 2001. 60:432–437.28. Tien YW, Yeh CC, Wang SP, Hu RH, Lee PH. Is blind pancreaticoduodenectomy justified for patients with ampullary neoplasms? J Gastrointest Surg. 2009. 13:1666–1673.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transduodenal Ampullectomy in Ampullary Neoplasm
- Safety of duodenal ampullectomy for benign periampullary tumors
- Endoscopic Ampullectomy for Tumors of the Ampulla of Vater: Long-term Follow-up Results
- Which one will you choose; open, laparoscopic, or robotic transduodenal ampullectomy?: a case report
- Robotic transduodenal ampullectomy: Case report and review of the literature